Pharmacy benefit managers (PBMs) and hospitals using the 340B program were in the crosshairs on May 17 as the House Energy & Commerce Health Subcommittee forwarded 17 bipartisan bills to the full committee.
The approved legislation included a package to increase transparency on pricing, strengthen critical public health programs, and secure access to care for low-income Americans. The subcommittee also discussed a comprehensive package to reauthorize and expand vital public health programs, and increase transparency for hospitals, health plans, and PBMs. In addition, the subcommittee advanced legislation to ensure Medicaid enrollees have access to breakthrough gene therapies, as well as reauthorize Animal Drug User Fee Amendments.
Here’s what you need to know about the legislation that moved forward yesterday.
PBMs in the hot seat
The PBM Accountability Act targets business practices of PBMs that drive up prices for patients, combining several earlier packages. It passed the subcommittee 27-0.
Rep. Stephanie Murphy (D-FL) said the Inflation Reduction Act (IRA) price controls go too far and PBMs are the real problem. She said about 50 drugs have been pulled from development thanks to overreach by the IRA.
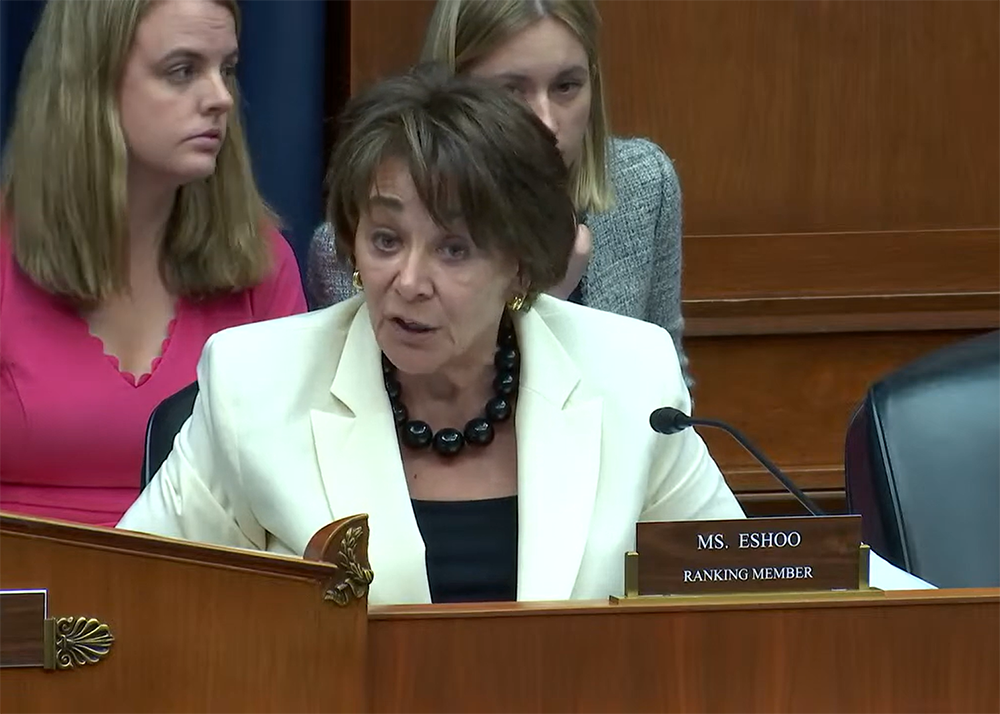
PBM abuses are “hurting people across the country. There isn’t any merit to this. …. Not any value added,” said Ranking Member Anna Eshoo (D-CA). “I can still hear my father’s voice: ‘Honey, it’s a racket.’”
PBMs need to be regulated, said witness Dr. Benjamin N. Rome of Harvard Medical School. Patients should not have to shop around for medicine; prices need to be reasonable from the start.
Large employers are not getting information from PBMs about money flow or the insurer’s rebates, explained witness Frederick Isasi, Executive Director of Families USA. Transparency is needed so the client (large employer) knows where the money flows, he said. PBMs should not be able to negotiate one price and then use a different price (the list price) for cost-sharing agreements with consumers, he concluded.
The subcommittee also approved H.R. 1613, the Drug Price Transparency in Medicaid Act of 2023.
H.R. 1613 is an amendment to Title XIX of the Social Security Act to improve transparency and prevent the use of abusive spread pricing and related practices in the Medicaid program. The bill requires pass-through pricing models, and prohibits spread-pricing, for payment arrangements with pharmacy benefit managers under Medicaid. The bill also extends funding for retail pharmacy surveys and requires additional information with respect to price concessions and survey participants to be made publicly available.
340B transparency
Some legislators were wary of moving forward on necessary 340B legislation, noting the program’s past success in helping underserved communities. Now, however, the 340B program has become bloated and abused by hospitals and others who take a profit. This has increased the value of pharmaceuticals subsidized under the program from $4 billion in 2009 to $43.9 billion in 2021, Bio.News reported.
Subcommittee Vice Chair Larry Bucshon (R-IN) said there needs to be transparency and there can be no growth without transparency. He cited the program’s rapid growth, noting it can be a “lucrative” business.
H.R. 3290 passed 16–12. The bill is an amendment to Title III of the Public Health Service Act to ensure transparency and oversight of the 340B drug discount program.
The next steps
These bills now go to the full House Energy & Commerce Committee. If passed by the committee, they move to the full House for a vote.
These were far from the only issues healthcare issues discussed, however. The breadth and bipartisanship of the markup bode well for future legislative steps to improve the transparency and affordability of healthcare.
Other bills to watch include:
- H.R. 1418, the Animal Drug User Fee Amendments of 2023, sponsored by Rep. Greg Pence (R-IN); passed 29–0.
- H.R. 2544, the Securing the U.S. Organ Procurement and Transplantation Network Act, sponsored by Rep. Bucshon (R-IN); passed 28–0.
- H.R. 2666, the Medicaid VBPs for Patients (MVP) Act, sponsored by Rep. Brett Guthrie (R-KY); passed 16–11.
- H.R. 3285, the Fairness for Patient Medications Act, sponsored by Rep. Morgan Griffith (R-VA); passed 27–0.
- H.R. 3284, the Providers and Payers COMPETE Act, sponsored by Rep. Michael Burgess (R-TX); passed 27–0.
- H.R. 2559, the Strengthening Community Care Act of 2023, sponsored by Rep. John Joyce (R-PA); passed 27–0.
- H.R. 2547, the Special Diabetes Program for Indians Reauthorization Act of 2023, sponsored by Rep. Tom Cole (R-OK), and H.R. 2550, the Special Diabetes Program Reauthorization Act of 2023, sponsored by Rep. Diana DeGette (D-CO); both passed 27–0.
- H.R. 2665, the Supporting Safety Net Hospitals Act, sponsored by Rep. Yvette Clarke (D-NY); passed 27–0.
- H.R. 3248, the Diagnostic Lab Testing Transparency Act, sponsored by Rep. Mariannette Miller-Meeks (R-IA); passed 27–0.
- H.R. 3262, To amend title XI of the Social Security Act to increase transparency of certain health-related ownership information, sponsored by Rep. Jan Schakowsky (D-IL); passed 27–0.
- H.R. 3282, the Promoting Transparency and Healthy Competition in Medicare Act, sponsored by Rep. Diana Harshbarger (R-TN); passed 27–0.
- H.R. 3237, To amend title XVIII of the Social Security Act to require each outpatient department of a provider to include a unique identification number on claims for services, and to require hospitals with an outpatient department of a provider to submit to the Centers for Medicare & Medicaid Services an attestation with respect to each outpatient department. This bill was sponsored by Rep. Joyce (R-PA) and passed 27–0.
Needless to say, it was a busy day, boding many more busy days to come.