Antimicrobial resistance (AMR) threatens our public health and economy, and legislation is required to address this threat, members of a July 25 bipartisan congressional roundtable agreed.
“We have the best physicians, the best facilities, the best technology, and everybody else has the technology we develop here, but we just can’t seem to put it all together,” said Rep. Jodey Arrington (R-TX), Chair of the House Budget Committee, whose Health Care Task Force organized the roundtable.
A critical piece of the puzzle that is urgently needed now would be bipartisan legislation like H.R. 2940, Pioneering Antimicrobial Subscriptions to End Upsurging Resistance (PASTEUR) Act, said participants—including Members of Congress and several AMR experts.
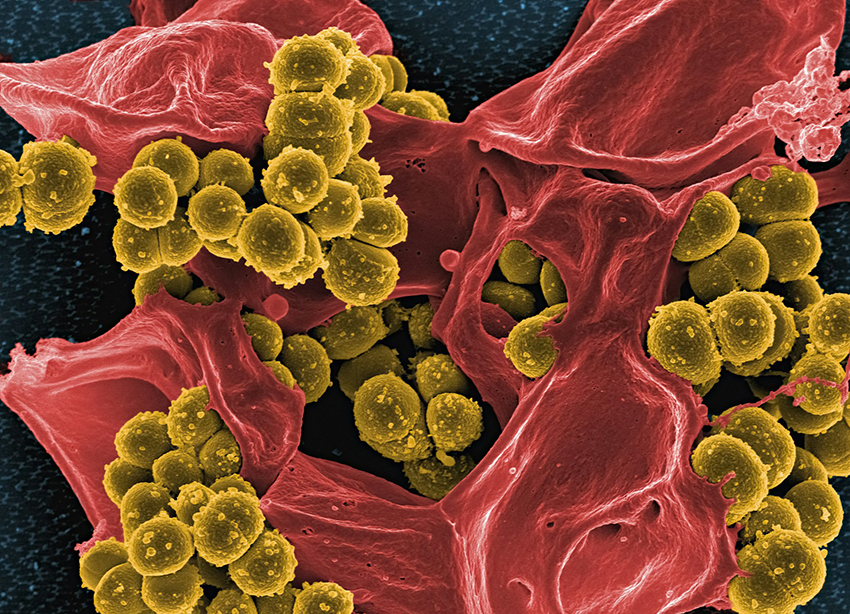
With drug-resistant “superbugs” contributing to nearly 5 million deaths annually, we need novel antimicrobial treatments to fight these infections. However, the market for these drugs is broken. The PASTEUR Act would help boost the antimicrobial pipeline by stabilizing a sustainable return on investment for new antimicrobials to treat the most threatening infections.
“We’ve been investing in AMR for a number of years, and there’s some great research being done. But then these innovative companies go bankrupt. Now, we have a bipartisan, bicameral bill moving. It’s important for America, and it’s important for the world,” said Rep. Drew Ferguson (R-GA), a co-sponsor of the PASTEUR Act, who participated in the roundtable.
The medical threat
“I would far rather practice in a time when antimicrobials are available than a time when they were not available,” said HCTF Chair Michael C. Burgess, M.D. (R-TX). “We are here tasked with safeguarding public health.”
In a July 25 editorial in Epoch Times, Rep. Ferguson noted the potential costs to health care.
“Should safe and effective antibiotics disappear, innovative medical treatments will need to be reconsidered—and decades of medical technology advancements that improve health outcomes of patients will be undone. The sheer size of the health system disruption that would occur without this infection prevention system will impact everyone,” he wrote.
“We know this problem is going to get worse,” continued Rep. Ferguson. “AMR already kills more people globally than HIV. How much longer should the United States wait before acting?”
The economic threat
During the roundtable, Rep. Scott Peters (D-CA), who co-leads the PASTEUR Act, explained the need for legislation.
“I believe in the market as a way to generate solutions for these things. But the market doesn’t work here. … You can’t induce investment into that risk, with no return. We are trying to figure out a way to make it make sense that people will create new antibiotics,” he said.
“But the other thing I think we’re up against is the way we budget,” Rep. Peters continued. “We must be willing to spend some money today to save money later and CBO (Congressional Budget Office) doesn’t always give us that mechanism. The cost is not this year’s money. But it’s this year’s money considering what we get back in future years. That’s an institutional problem that we have. We have to deal with this.”
Ferguson’s Epoch Times editorial further elucidated the potential costs of AMR.
“Every year, antibiotic-resistant infections are estimated to cost the U.S. economy $20 billion in direct health care costs and an estimated $35 billion in lost productivity. These costs are ultimately borne by patients, as resistant infections add nearly $1,400 to their overall health care costs,” Rep. Ferguson wrote.
“Yet the most substantial costs will occur when doctors no longer follow the medical standards for patient care,” he explained. “Cancer doctors will be hard pressed to recommend chemotherapy without the antibiotics to protect their patients from infection. Many surgical procedures will be too risky to perform. The costs associated with rethinking new medical standards are incalculable.”
BIO support for the PASTEUR Act
The Biotechnology Innovation Organization (BIO) is one of more than 230 organizations—from industry, health care, research, and biopharma—supporting the PASTEUR Act in a letter to Congress last year. BIO has continued its advocacy for the legislation.
“This bipartisan bill would help align market incentives with critical innovation by establishing an alternative payment model for antimicrobials to treat the most threatening infections,” Emily Wheeler, BIO Senior Director, Infectious Disease Policy, has explained. “Under this system, the government would enter into contracts with innovators to pay for consistent access to novel antimicrobials with payments that are decoupled from the volume of antimicrobials used.”
Phyllis Arthur, BIO’s EVP and Head of Healthcare Policy and Programs, has called for passage of the PASTEUR Act in testimony before Congress.
The proposed legislation “enables a marketplace for these products that are being developed by industry, sometimes in partnership with [the Biomedical Advanced Research and Development Authority] and the government,” she testified. “And so we need to have these products not just get developed, but go into a place where they can actually be sustained and be available to us.”