As part of our coverage of the National Institute of Health’s (NIH) Innovation Zone at the 2023 Biotechnology Innovation Organization (BIO) International Convention, Bio.News spoke with Quivive Pharma Founder and CEO, John Hsu, M.D.
Quivive is focused on addressing the opioid epidemic and bringing hope to those impacted through innovation in oral medication and respiratory treatment.
The following has been edited for length and clarity.
Bio.News: The opioid epidemic has devastated countless communities in the United States and abroad. How did the epidemic inform Quivive Pharma’s creation and continued growth?

Dr. Hsu: The process for creation of Quivive started 30 years ago. As an anesthesiologist and pain management and addiction medicine physician, I was on the front lines of the opioid epidemic. I watched the problem go from an opioid problem, then to a crisis, and subsequently to an epidemic.
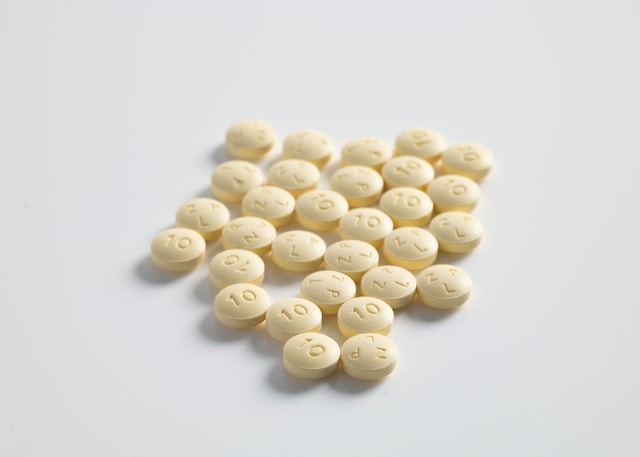
To make current opioids better, safer, and abuse-deterrent, I added a U.S. Food and Drug Administration (FDA)-approved respiratory stimulant that could support breathing and deter abuse. We are going about development with two great partners: the National Institutes of Health’s (NIH) National Institute on Drug Abuse (NIDA) and the Cleveland Clinic.
Knowing the issues about the lack of medication adherence and lack of opioid security led me to the iPill dispenser. iPill consists of a pill dispenser operated by a mobile app for secure opioid storage, real-time remote medication adherence monitoring with bidirectional alerts for missed dose detection and remediation, biometric active controlled dispensing, and secure storage with destruction of unused pills if tampered with, and automatic destruction at the end of 30 days.
Many patients with opioid use disorder (OUD) are limited by education, income, social determinants of health (SDOH), health literacy, and access to OUD treatment. iPill is trying to address these issues with technology by bringing medications to them. iPill can be prefilled with medications for opioid use disorder (MOUD) and sent directly to patients’ homes.
Bio. News: What has the challenge of abuse deterrents of opioids been historically and how is Quivive Pharma working to address that challenge more effectively?
Dr. Hsu: Quivive addresses many of the issues of opioid use disorder. Quivive balances safety of opioids with efficacy of pain treatment with opioids. By making the oral pill in combination with the respiratory stimulant inseparable, pain can be treated efficaciously. Should more than the prescribed dose be taken, the two potentially lethal side effects are addressed by the respiratory stimulant. In effect, Quivive begins safety and preventative measures when the opioid is taken—not after problems develop.
Treating patients in acute pain is a first step to address the opioid crisis. Furthermore, secure storage of opioids at home is not the norm at this time. Monitoring medication adherence is not the norm at this time, despite the fact that 50 percent of patients take drugs incorrectly and not as prescribed. Quivive has recognized a path forward in this complicated situation with many variables.
Bio.News: Could you please elaborate on Quivive Pharma’s “Functional Antagonism” model of opioid use and deterrence, and what makes it both particularly effective and unique?
Dr. Hsu: Quivive Pharma’s “Functional Antagonism” model of opioid use and deterrence works, because two different drugs are working on two different receptors for respiratory control. Opioids work on the mu receptor to relieve pain and depress respiration. The opioids would stimulate relief of pain and depress respiration, and Doxapram would stimulate respiration.
Relief of pain would continue because Doxapram exhibits no action on the mu receptor. The balance of safety and efficacy of an opioid and respiratory combined and inseparable drug swings in favor of the opioid becoming safer. Both opioids and the respiratory stimulant Doxapram are known FDA-approved drugs.
Regarding the abuse deterrence, Quivive adds a sub-therapeutic dose in a ratio to the opioid, so as to not cause a clinical effect. At overdose levels, the respiratory stimulant will accumulate to a clinically effective dose. So by adding the respiratory stimulant to the opioid, we create a functional antagonism model to support respiration in the face of opioid-induced respiratory stimulation and deter abuse with the fight-or-flight response to high near-overdose levels of the respiratory stimulant.
Bio.News: What does the future look like for Quivive Pharma? Is there any end in sight when it comes to the American issue of pain and pain-related addiction?
Dr. Hsu: The future of Quivive looks bright. We have two great partners in NIH’s NIDA and the Cleveland Clinic to support our rapid development. Once we submit the NDA and obtain FDA approval in 2025, we can address and treat many patients who are suffering in pain today. Quivive products will be cost-effective (Tier 1 generics), improve the treatment of pain with fewer overdoses and fewer OUD patients, and reduce the cost of healthcare in the U.S.
We must treat pain. We must do it safely and efficaciously and deter abuse. We must prevent the predominance of OUD from taking over our youth.
Regarding American issues of pain and pain-related addiction, all the stakeholders must come to a consensus. I think we are missing the human factor in the opioid epidemic. We must treat pain, and we need to improve access to OUD. We need holistic treatment of the mind and the body with psychosocial support (CBT, ACT, CM) and physical support with MOUD. It must be immediately accessible and on demand so it has the best chance to reduce cravings, withdrawal symptoms, relapse, and overdose.
For the opioid epidemic, we need to treat pain, treat OUD, and all get behind these needs. We cannot restrict access to pain medications because they cause respiratory depression and addictions—we can make them better.