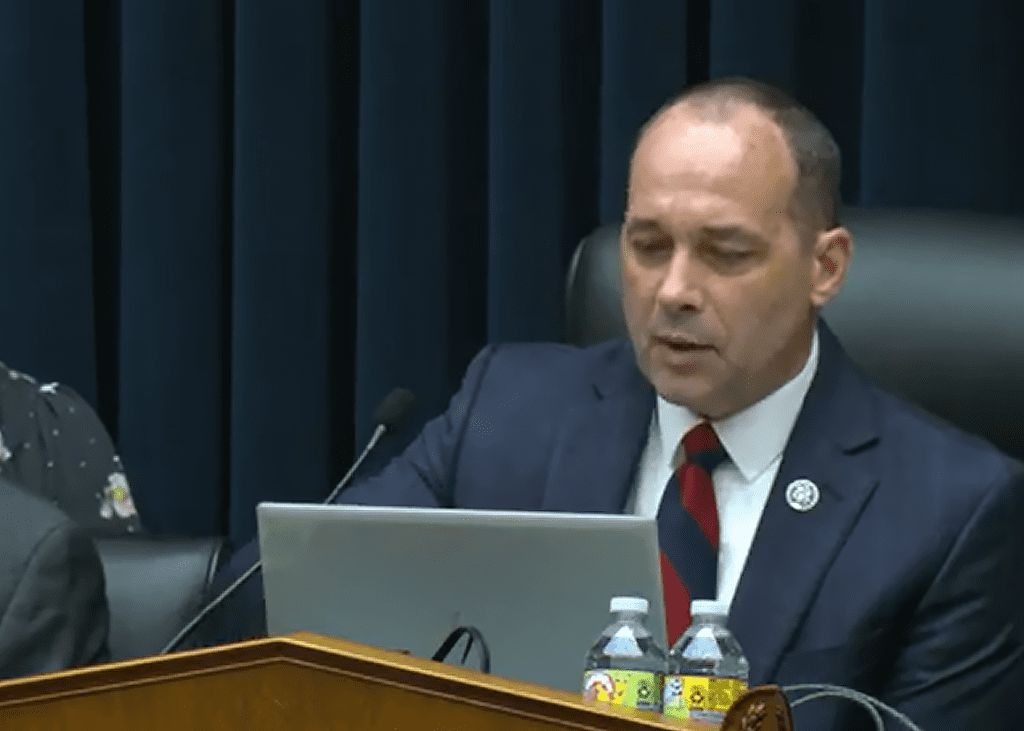
A June 21 House hearing on health care costs put a sharp focus on the need for transparency to prevent pharmacy benefit managers (PBMs) from driving up the price of prescription drugs.
Experts at the House Committee on Education and the Workforce Subcommittee on Health, Employment, Labor, and Pensions hearing laid out the ways in which PBMs benefit by raising costs for patients and reducing revenue for drug makers. In response, Congress members from both parties called for legislation to stop the abuses by shining light on the practices of PBMs.
PBMs determine the formulary of drugs that insurers will cover, and demand rebates from drug makers in exchange for this coverage. While PBMs are supposed to pass on the savings from these rebates to insurers and patients, research shows they pocket those savings as profits—though it’s hard to know how much PBMs profit.
The PBMs “operate in a black box,” said Subcommittee Chair Bob Good (R-VA). “Nobody knows the details of the rebate deals they negotiate with drug manufacturers, creating perverse incentives for PBMs to choose more expensive drugs with larger rebates.”
Consolidation a concern
Rep. Good noted that 80% of the market is controlled by three PBMs who are “subsidiaries of Fortune 500 health care companies that also own insurers, pharmacies, and—most recently—physicians, giving them even more influence over prescription benefits.”
The big three PBMs are: CVS, including Caremark and Aetna; Express Scripts owned by Cigna; and Optum owned by UnitedHealth Group, said witness Sophia Tripoli of the Center for Affordable Whole-Person Care, Families USA.
She recommended legislation to regulate PBM consolidation while also “allowing plans and employers to receive data on negotiated rates, gross PBM profits, cost-effectiveness of the PBM’s drug list and spending patterns.”
Rep. Good said better access to information would keep PBMs honest. “If they truly passed rebate savings to consumers—like PBMs say they do—this would be a non-issue,” he said. “Without transparency, the PBM business model is ripe for abuse.”
Examples of PBM windfalls
When PBM practices are investigated, they reveal the level of profits being taken.
“A Delaware state auditor report found Express Scripts overcharged the state employee prescription drug plan by $24.5 million,” Tripoli said. She added that the Ohio Department of Health “found that CVS Caremark and Optum Rx pocketed the nearly 9% difference between what they billed managed care plans and what they paid pharmacies instead of passing those savings on to families.”
Another witness, Greg Baker of AffirmedRx, said that Mark Cuban’s direct-to-consumer pharmacy, which avoids the PBM model, offers a year’s supply of the cancer drug Imatinib for $866. “However, when PBMs negotiate Imatinib prices for state-run health plans in states like Kentucky, Louisiana, Georgia, or Tennessee, a year’s supply costs $26,000, $57,000, $170,000, and $212,000, respectively,” according to a hearing recap.
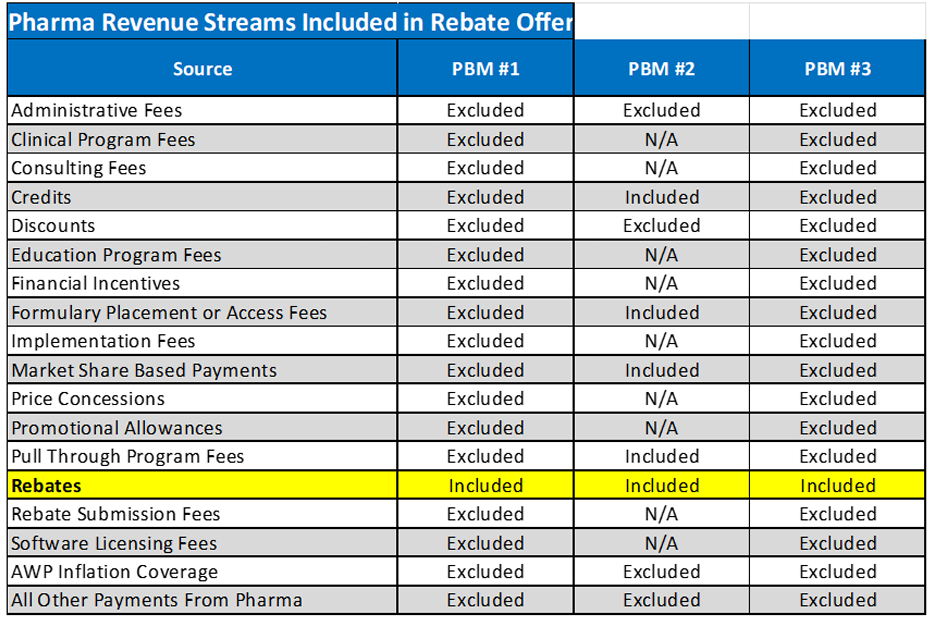
Baker noted that the money PBMs take from drug makers are not just from rebates but also from an extensive list of fees that provide revenue. He offered a breakdown of how much of those fees are listed as rebates by three unnamed PBMs.
Small businesses suffer
Along with highlighting the impact on patients, Congress members at the hearing noted the damage to businesses caused by the problem.
Rep. Tim Walberg (R-MI) said he is constantly hearing from small business owners about “the disconnect” between the cost of drugs from drug makers and the cost to employers and patients.
In her opening statement, Virginia Foxx (R-NC), Education and the Workforce Committee Chairwoman, said: “Health care cost is the number one issue facing small businesses today. In fact, according to the NFIB (National Federation of Independent Businesses), it has been their top issue for over 30 straight years.”
One kind of small business hurt by the situation is independent pharmacies, according to Susan Wild (D-PA). She asked why PBMs can access medicines when small pharmacies can’t. Baker explained that vertical integration means chain pharmacies have better supplies.
The current model means “small local, independent pharmacies are almost a thing of the past,” said Wild. “Many of them have closed, much to the sadness and detriment of consumers around my district, who had personal relationships with their local pharmacist.”
Rep. Kathy Manning (D-NC) asked about how to improve reimbursement from PBMs and Rep. Bobby Scott (D-VA) questioned the impact on patients’ out-of-pocket costs for their prescriptions.
Solution: Transparency
The solution would be legislation to open up the “black box,” revealing all the data about PBM profits, and the savings they should pass on, said experts and Congress members.
“Corruption thrives in darkness, and as a conservative, I believe that for good governance, we ought to strive for more transparency,” said Rep. Good.
“As a progressive, I agree with you. I believe in transparency,” said Ranking Member Mark DeSaulnier (D-CA). “We should all agree that employers and consumers deserve to know how the rebates PBMs receive from drug manufacturers impact their decisions that raise costs for workers and families.”
The lack of transparency “limits our ability as policy makers to improve our healthcare system” said Rep. DeSaulnier. He added that once transparency was achieved, the next step is to change the system with new policy. “I also hope to explore ideas for changing the incentives for PBMs, to make sure they act in the best interest of clients.”
Subcommittee members promised that there will be additional hearings and work on the subject as they seek solutions to providing affordable prescription drugs, and health care in general.