In a new report, Preparing for the Next Pandemic in the Era of Antimicrobial Resistance, the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria (PACCARB) outlined measures for pandemic preparedness amidst the rising threat of antimicrobial resistance (AMR), which could contribute to future viral or bacterial pandemics.
Aside from recent alarming rates of infections, including nearly 1.27 million global deaths attributed to bacterial infections in 2019, PACCARB emphasizes the need for revised pandemic policies, considering the challenges faced by the U.S. during the COVID-19 pandemic.
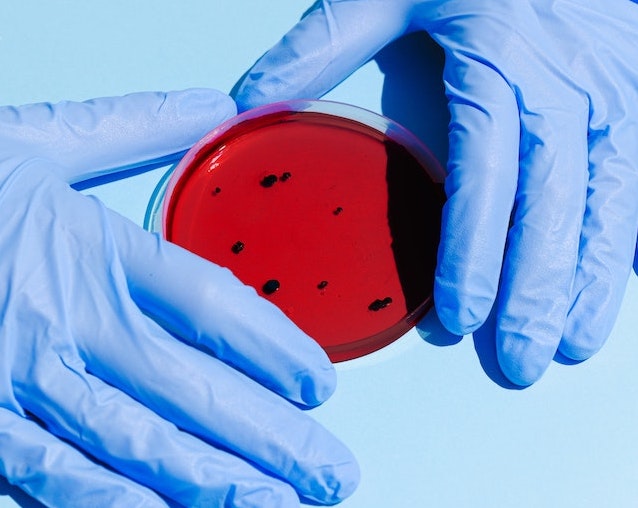
Bacterial infections lay at the heart of many illnesses, making them a leading cause of complications during delicate health circumstances. For instance, hospitalized COVID-19 patients faced substantial morbidity and mortality caused by drug-resistant infections.
Alongside health-related developments, PACCARB highlights flaws within the medical infrastructure. Examples include staffing shortages, limited availability of supplies and medications, and a lack of resources and funding for AMR activities.
How should we address AMR?
PACCARB recognizes four major areas of change to better prepare for and combat antimicrobial resistance, whether during daily life or public health emergencies. These include:
- Infection prevention and control and antimicrobial stewardship, including integration of these otherwise absent subjects into U.S. pandemic policymaking.
- Workforce expansion. Updated policies related to staff training and support for a more efficient working environment are needed.
- Data sharing and security. This includes gathering AMR surveillance data from a variety of subjects and their environments, including humans, animals, and plants.
- Product innovation and development (medical countermeasures), especially to prepare for public health emergencies.
These improvements aim to provide a more equitable distribution of resources among communities while facilitating a more coordinated and efficient response to AMR and public health emergencies.
The urgency for policies surrounding antimicrobial resistance has become increasingly important as new findings of AMR start to integrate into our everyday lives.
For instance, antibiotic-resistant bacteria was found in Los Angeles County’s wastewater for the first time ever in early April. It was discovered by Professor Adam Smith from the Sonny Astani Department of Civil and Environmental Engineering at the University of Southern California.
“We are propagating antibiotic-resistant bacteria,” says Smith, explaining the sudden increased use of antibiotics during the pandemic has played a pivotal role in the increased resistance.
Former Biotechnology Innovation Organization (BIO) President and CEO Dr. Michelle McMurry-Heath discusses the significance of AMR in an episode of the I am BIO Podcast. “Existing antibiotics could stop working altogether in the near future,” she says.
While the battle against antimicrobial resistance continues, the notable takeaways from the voices of entities across the world remain the same—urgent need for changes in policy and preventative measures.
As PACCARB stresses, this pivotal moment should be taken as an opportunity to rethink, revise, and rebuild from our experiences and address the growing gaps in our healthcare infrastructures.
Their key advice: “By investing in creating a more resilient health system while keeping the community involved in the process, emergency policies will be more effective and efficient when deployed to fight the next PHE (public health emergency).”