A new antibiotic that could potentially be effective against many superbugs, tuberculosis, and even “untreatable” illnesses has been discovered, reports Nature, using none other than the talk of the year itself: AI.
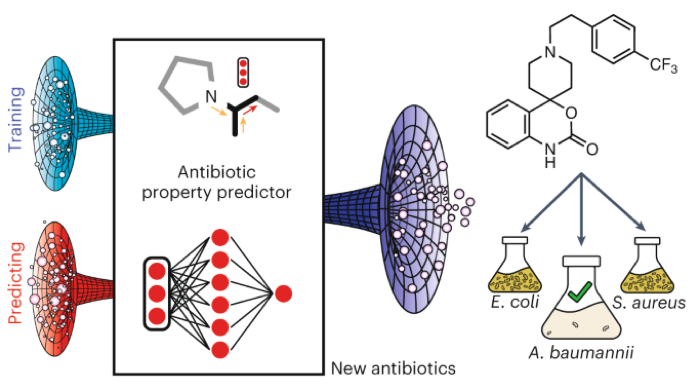
Using artificial intelligence (AI), researchers successfully narrowed down a handful of chemicals from a library containing almost 7,000 potential compounds. This resulted in an effective experimental antibiotic called abaucin, which if developed, could be used to fight Acinetobacter baumannii, a bacteria that is known to cause serious infections like meningitis and pneumonia.
According to Jonathan Stokes, Assistant Professor of Biochemistry and Biomedical Sciences at McMaster University, A. baumannii isolates are resistant to almost every antibiotic, as “Acinetobacter can survive on hospital doorknobs and equipment for long periods of time, and it can take up antibiotic resistance genes from its environment,” MIT quotes Stokes as saying.
James Collins, the Termeer Professor of Medical Engineering and Science in MIT’s Institute for Medical Engineering and Science (IMES) and Department of Biological Engineering, praises AI, expressing his excitement about the plethora of opportunities machine learning can offer.
“This finding further supports the premise that AI can significantly accelerate and expand our search for novel antibiotics,” Collins says, per MIT.
But what if we could skip antibiotics?
At Shank Lab, Elizabeth Shank, Associate Professor of Systems Biology, focuses on developing new antibiotics derived from compounds made by soil bacteria.
According to Shank, bacteria and other microbes use chemical cues to communicate, or “talk,” so by intentionally growing these species together, the lab is hoping the bacteria “interaction” will lead to new compounds.
Shank says that if they’re able to stimulate new chemical cues by predicting the bacterial interactions, they may be able to change a pathogen’s phenotype or behavior—thus eliminating the need to use antibiotics.
“We want to exploit these chemical signals that bacteria are already using to communicate with each other so that we can manipulate their behavior, prevent disease, and reduce antibiotic use. If we can identify these chemical signals that eliminate biofilms or that prevent other harmful pathogenic phenotypes associated with different diseases, we could use these compounds as drugs to improve human health,” says Shank, per UMass Chan.




