Artificial intelligence (AI) is revolutionizing drug discovery, paving the way for groundbreaking treatments. In fact, a recent study found that biotech companies using AI have developed over 150 small molecule drugs in development, and there are two dozen or more AI-designed drugs in or entering clinical trials.
But as more of these treatments advance to later-stage trials, there’s growing interest in better understanding the process. What led AI to select that particular target? How exactly did generative AI design a new molecule—and how can we be sure that it will be effective?
A technological breakthrough
A new paper in Nature Biotechnology from biotech company Insilico Medicine helps to shed light on this process, revealing the journey behind a lead AI drug known as INS018_055 with enough data to satisfy even the most curious minds. The drug is designed to combat a rare lung disease called idiopathic pulmonary fibrosis (IPF), which affects 5 million people worldwide, and it is the first AI-designed drug for an AI-discovered target to reach Phase II trials with patients.
While the drug’s advancement into later-stage trials represents hope for patients—who currently have limited treatment options and none that stop the disease or reverse its effects—it also provides an opportunity to share exactly how this technological breakthrough works.
“Nowadays, it seems that we read about the virtues of AI, machine learning, and generative design almost daily,” says Stevan Djuric, Ph.D., adjunct professor in medicinal chemistry at the University of Kansas and former head of the global medicinal chemistry leadership team at AbbVie. “There is a feeling that, perhaps, it is overhyped. However, in this paper, the Insilico Medicine team convincingly demonstrates the power of their proprietary platform which features target identification and validation, medicinal chemistry design and clinical trial components using the aforementioned tools.”
AI is not bound by what’s been done before. It can comb through complex scientific datasets and find unique approaches to solving problems that have long challenged scientists.
“As a clinician, I see firsthand the need for novel, effective treatments,” says Christoph Kuppe, Ph.D., a physician scientist at RWTH Aachen University in Germany. “This landmark work highlights the central role that AI can play in accelerating the path from discovery to treatment, reshaping our strategy against diseases that currently have limited therapeutic options.”
TNIK—targeted through AI discovery
In the case of this lead drug, the Insilico team used numerous datasets related to lung fibrosis from the National Center for Biotechnology Information’s Gene Expression Omnibus (GEO) database—an international public repository of genomics data submitted by the research community—and tasked its AI target discovery engine, PandaOmics, with finding a new way to inhibit this disease.
The AI zeroed in on a protein kinase called TNIK—known to play a role in colorectal cancer and lung cancer but never previously explored for fibrosis.
“When we started the preclinical profiling of INS018_055 for fibrotic diseases, everybody was seeing its target TNIK as a candidate for oncology indications,” says Klaus Witte, M.D., a German Medical Board-certified pharmacologist and toxicologist who served as a preclinical consultant on the drug. “Although I was skeptical in the beginning, all data that we generated clearly supported Insilico’s prediction of anti-fibrotic efficacy.”
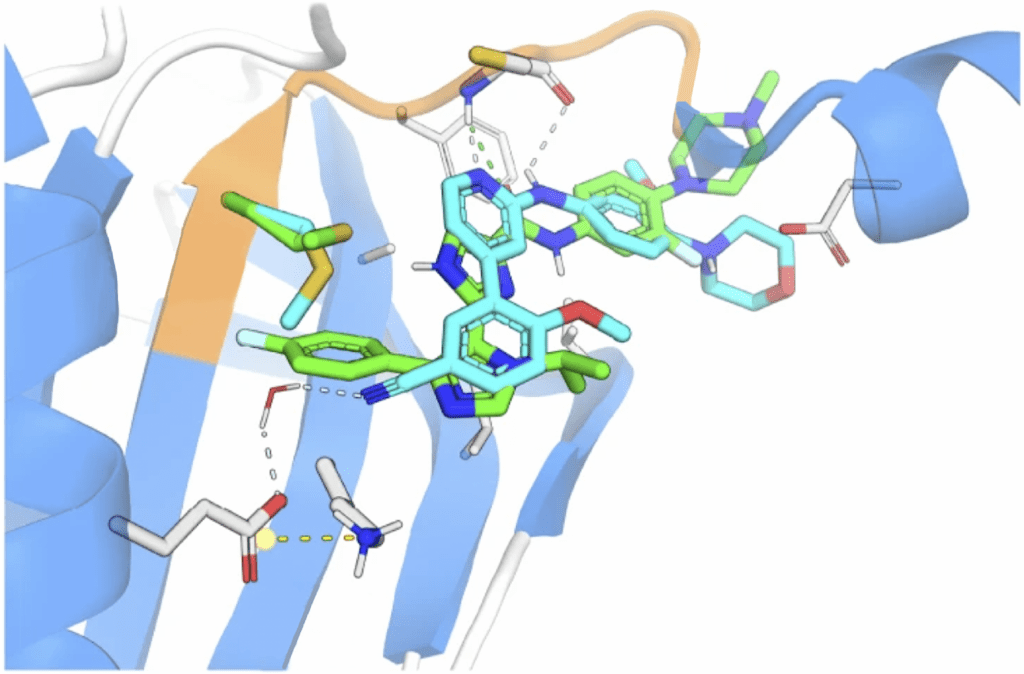
So the team persisted, and began the process of designing a new molecule, beginning with the known crystal structure of the TNIK kinase. They then directed the generative AI engine, Chemistry42, to make small molecules that could bind to this structure in a unique way.
Djuric mentions that when it comes to designing molecules, medicinal chemists are not as interested in improving the potency of compounds as they are in fine tuning a drug’s off-target effects. The paper demonstrates how AI designs highly optimized molecules that offer synthetic accessibility, novelty, and desired medicinal chemistry properties much more quickly than traditional methods—in this case, just 18 months from target identification to preclinical candidate.
The future of drug development
A McKinsey study found that AI could more than double improvement in lead optimization—or selection of a lead drug candidate—through faster experiments and faster compound design. These gains are critical to improving the sluggish success rate of pharmaceutical development. It still takes a decade or more to bring a drug to market, costs over $2 billion per drug, and over 90% of these drugs fail in clinical trials.
With positive results in early trials with healthy volunteers, the lead drug has now advanced to phase 2a clinical trials with IPF patients in the U.S. and China to further test its safety, tolerability, pharmacokinetics and preliminary efficacy, including how this drug impacts lung function.
IPF treatments on the market are largely tyrosine kinase inhibitors—including nintedanib, imatinib, and nilotinib. These approved therapies may offer some relief or slow progression, but they do not reverse damage or stop the disease, and they can bring unpleasant side effects like nausea and stomach pain.
This is the first IPF drug in development that is designed to work by inhibiting TNIK—a novel drug designed by AI for a novel target discovered by AI. It’s an important moment.
“There has been much speculation that AI and deep learning methods will have a substantial role in shaping the future course of drug development,” says Charles Cantor, Ph.D., professor emeritus at Boston University and former Chief Scientific Officer of Sequenom, who is on Insilico’s Scientific Advisory Board. “This paper presents a very convincing proof of concept. Driven by AI at nearly every stage from target identification, to drug candidate selection, to Phase 1 studies, a novel molecule is now ready for Phase 2 clinical trials. If this process proves to be general, drug development without AI may well become inconceivable.”