Antimicrobial resistance (AMR) presents a clear threat to human health and healthcare systems. And in the post-COVID era, the threat and calls to address the issue have increased.
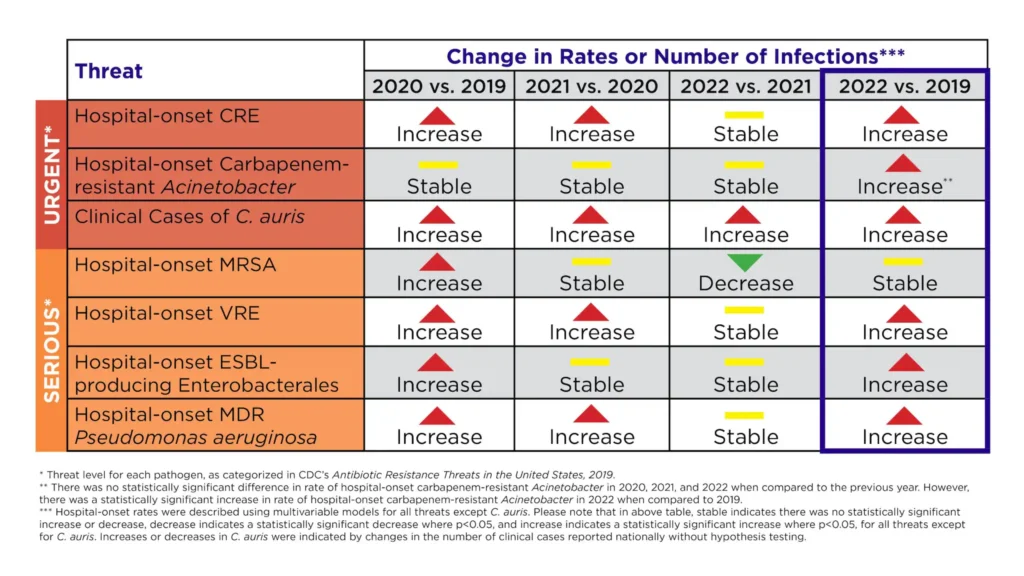
On July 16, the Centers for Disease Control and Prevention (CDC) released a new fact sheet, Antimicrobial Resistance Threats in the United States, 2021-2022. And the findings are concerning. According to the fact sheet, which studied seven different AMR pathogens typically found in healthcare settings, the onset of AMR pathogens increased “by a combined 20% during the COVID-19 pandemic compared to the pre-pandemic period, peaking in 2021.”
The trend has continued in the post-COVID era. In 2022, all but one of the studied AMR pathogens remained above pre-pandemic levels.
One AMR pathogen has been increasing the most: Candida auris (C. auris)
“The number of reported clinical cases of C. auris increased nearly five-fold from 2019 to 2022,” writes the CDC. That being said, each of the AMR pathogens studied posed either a serious or urgent threat to healthcare systems today.
COVID’s impact on AMR
One of the more interesting findings in the data is that COVID had a discernible effect on the increase in AMR burden in hospitals, “which pushed healthcare facilities, health departments, and communities near their breaking points,” the CDC explains.
Contributing factors include the increased amount of time patients spent in hospitals due to COVID infections, as well as the influx of patients burdening hospitals during the pandemic. The sharp influx of patients “challenged the implementation of infection prevention and control practices, and increased inappropriate antibiotic use,” notes the CDC.
What biotech is doing to address AMR
With drug-resistant “superbugs” contributing to nearly 5 million deaths annually, we need novel antimicrobial treatments to fight drug-resistant infections. However, the market for these drugs is broken.
“Antimicrobial resistance truly is one of the leading public health threats of our time,” Emily Wheeler, BIO’s Senior Director of Infectious Disease Policy, told the Los Angeles Times. “The pipeline for antibiotics today is already inadequate to address the threats that we know about, without even considering the continuous evolution of these bugs as the years go on.”
According to a recent analysis of the antibacterial pipeline by the World Health Organization (WHO), there are only four innovative antibiotics in development for the “critical priority pathogens,” which are designated as the highest risk by WHO.
“Overall, antibacterial agents in the clinical pipeline combined with those approved in the last six years are still insufficient to tackle the ever growing threat of the emergence and spread of drug-resistant infections,” says the report. Meanwhile, the workforce in AMR research and development has been significantly declining over the past two decades. A recent report by the AMR Industry Alliance found “the number of authors on all AMR publications declined from a high of 3,599 in 1995 to just 1,827 in 2020.”
How policy can support antimicrobial development
A legislative proposal under consideration on Capitol Hill could help. The PASTEUR Act would help boost the antimicrobial pipeline to bring new innovations to patients by stabilizing a sustainable return on investment for new antimicrobials to treat the most threatening infections. The legislation was reintroduced in Congress in April 2023 with clear calls for passage among policymakers and stakeholders.
“Right now, we don’t have the tools to address the threat posed by antimicrobial resistance—and infectious disease experts are warning us that it will only get worse,” said Sen. Michael Bennet (D-CO), who co-sponsored the reintroduced bill. “The bipartisan PASTEUR Act is the strongest bill ever written to strengthen antibiotic development and use. It will fix our market failures, expand the pipeline for next generation antibiotics, and save lives.”
The new findings released from the CDC show an extensive increase in the burden of AMR pathogens on the U.S. healthcare system.
“This latest data from the CDC is a striking reminder of the rapidly growing threat we face from antimicrobial resistance and further demonstrates why we need new, innovative therapies to address drug-resistant infections,” said Emily Wheeler after reviewing the data. “We need urgent action on the PASTEUR Act to help address the broken antimicrobial ecosystem and support the development of new tools to protect patients from these dangerous infections.”