The Biotechnology Innovation Organization (BIO) hailed inclusion of a bill to encourage new treatments for children with rare diseases and measures targeting reform of pharmacy benefit managers (PBMs) in the package of legislation passed Feb. 3.
The Mikaela Naylon Give Kids a Chance Act, reauthorizing the Pediatric Priority Review Voucher (PPRV) until 2029, was attached to the spending package that ended a partial government shutdown. The package also included legislation to prevent PBM compensation from being linked to the list price of a drug and measures to increase PBM transparency.
PPRV ‘provides critical incentives’
“The passage of the Mikaela Naylon Give Kids a Chance Act is a bipartisan victory for children and families living with rare diseases,” said a statement from BIO President & CEO John F. Crowley. “The PPRV program provides critical incentives for rare disease research, and its reauthorization provides stability and confidence for biotech innovators who are leading the way in the discovery of breakthrough treatments.”
First launched in 2012, the PPRV program gives vouchers to drug makers who gain Food and Drug Administration (FDA) approval for a treatment targeting a rare disease that affects children. The voucher grants expedited review of any future drug that the drug maker brings for FDA approval. The voucher can also be sold to fund research.
While the program costs taxpayers nothing, the vouchers have proven to incentivize drug makers, for whom early approval means an earlier opportunity to start earning revenues from years of research.
According to a new study from the National Organization for Rare Disorders (NORD), since the program’s inception in 2012, there have been 63 vouchers awarded for drugs targeting 47 different rare pediatric diseases. Before the PPRV program, only four of these 47 rare pediatric diseases had any FDA-approved treatments.
The program had been reauthorized every few years since it started in 2012, but was allowed to expire in 2024 and only reauthorized on Feb. 3.
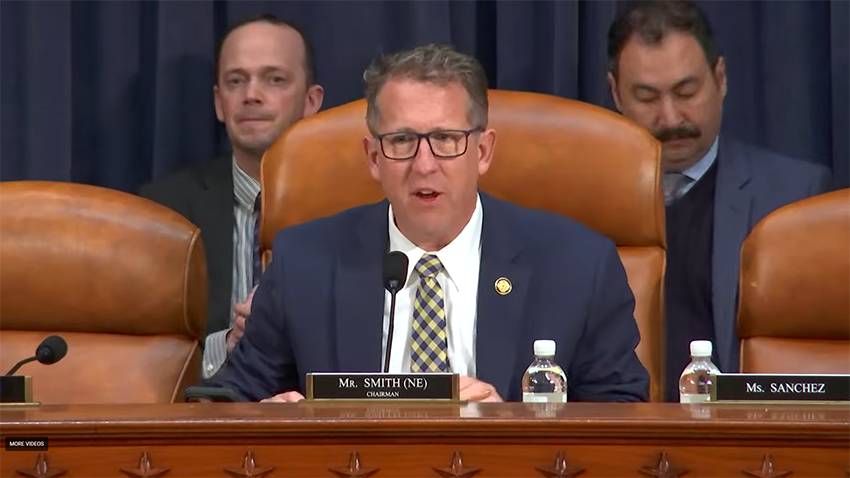
Aiken Hackett, BIO SVP of Federal Government Relations, noted the many people who joined BIO in pushing for reauthorization. “Our ultimate success was achieved through the bipartisan commitment of congressional champions, committee leadership and members of Congress committed to this program. Without them, and the dedicated patient advocates and organizations, hope for children and families touched by rare disease would be lost,” Hackett said.
Crowley also thanked the patient advocates who have been pushing for PPRV reauthorization and praised the lawmakers behind the bill. These included the chairs and ranking members of the House Committee on Energy and Commerce, the Senate Finance Committee, and the Senate Health, Education, Labor & Pensions (HELP) Committee.
Crowley noted the contributions of Senators Markwayne Mullin (R-OK) and Michael Bennet (D-CO), and Representatives Michael McCaul (R-TX), Debbie Dingell (D-MI), Gus Bilirakis (R-FL), Kim Schrier (D-WA), Diana Harshbarger (R-TN), Doris Matsui (D-CA), Dan Crenshaw (R-TX), Kathy Castor (D-FL), Randy Weber (R-TX), and Lori Trahan (D-MA).
PBM reforms on pricing, transparency
“This funding package also takes important first steps to rein in Pharmacy Benefit Managers (PBMs),” Crowley said. “For too long, these middlemen have driven up costs for patients.”
Three PBMs control 80% of all U.S. prescriptions and use their market power to profit while raising drug prices and reducing patient access, as Bio.News has reported for several years. PBMs’ grip on the market is even stronger because they are owned by corporations that also own insurance companies, pharmacies, and even medical practices.
“As a result of this high degree of consolidation and vertical integration, the leading PBMs can now exercise significant power over Americans’ access to drugs and the prices they pay,” said a report by the Federal Trade Commission (FTC).
One of the reforms passed Feb. 3 prevents PBMs from linking the remuneration they receive for drugs covered by Part D to the price of the drug, according to a statement from Rep. Earl “Buddy” Carter (R-GA). This measure addresses a system that encouraged PBMs to raise the price of drugs in order to receive greater compensation.
Other PBM reforms in the legislation target transparency. One provision, requires PBMs to provide group health plans with data on prescription drug spending and how much PBMs share of rebates they receive from drug manufacturers.
The legislation also contains measures to ensure PBMs are dealing more fairly with independent pharmacies, Carter’s statement explained.
“It is time to simplify our health care system, cut out the middlemen, and reduce out-of-pocket costs for patients,” said BIO’s Crowley. “We look forward to continuing to work with Congress and the Administration to realize a 21st-century vision for healthcare access and affordability for American families.”