During the COVID-19 pandemic, drug-resistant infections and resultant fatalities increased in hospitals by 15%, erasing years of progress in the United States in the fight against drug-resistant diseases, according to a new report issued by the Centers for Disease Control and Prevention (CDC) on Tuesday.
The study estimates that more than 29,400 individuals died from antimicrobial-resistant (AMR) infections in 2020. Given that data for half of the 18 pathogens designated as risks is unavailable or delayed, the actual number is likely significantly higher.
Over 40 percent of these deaths occurred in hospitalized patients who contracted the coronavirus.
Between 2012 and 2017, AMR-related fatalities fell 18% overall and nearly 30% in hospitals. However, in 2020, deaths from hospital-acquired superbugs increased 15%.
“This setback can and must be temporary. The COVID-19 pandemic has unmistakably shown us that antimicrobial resistance will not stop if we let down our guard; there is no time to waste,” said Michael Craig, MPP, Director of the CDC’s Antibiotic Resistance Coordination & Strategy Unit. “The best way to avert a pandemic caused by an antimicrobial-resistant pathogen is to identify gaps and invest in prevention to keep our nation safe.”
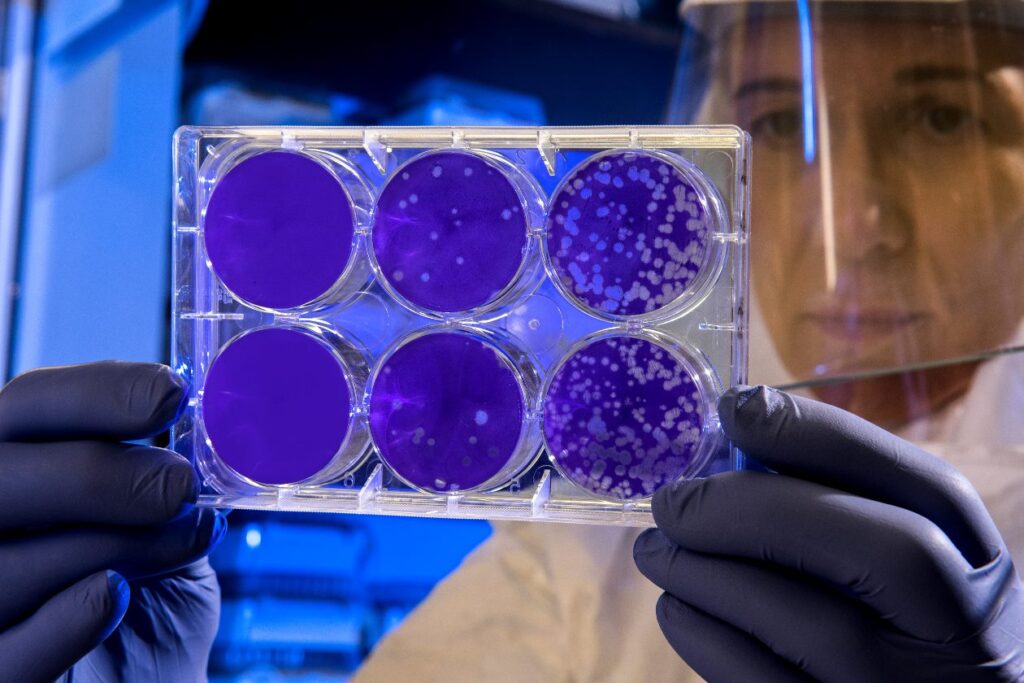
Specifically, the CDC found that dangerous bloodstream and urinary tract infections from Carbapenem-resistant Acinetobacter rose by 78%, while hospital infections rose for deadly superbug yeast Candida auris (60%) and “nightmare bacteria,” Carbapenem-resistant Enterobacteriaceae (35%). In addition, 3 of 5 resistant bacteria and fungi saw increased hospital infections.
The CDC says it was a “perfect storm”: hospitals treated ill patients with ventilators and catheters, which breach the body’s protective barriers and allow infection to spread.
Doctors used antibiotics extensively, but because COVID-19 is a virus, they had no impact. Antibiotic overuse increases drug-resistant bacteria. Because data gathering was delayed, illnesses went undiagnosed and untreated. Overburdened hospitals stifled progress in AMR prevention.
The CDC intends to prioritize infection control training, initiatives to regulate how antibiotics and antifungals are given and used, treatment research, tracking infections in the community using wastewater or sewage, and extending data networks.