On July 17, Eli Lilly announced positive results from clinical trials of donanemab, the company’s candidate for the treatment of Alzheimer’s disease.
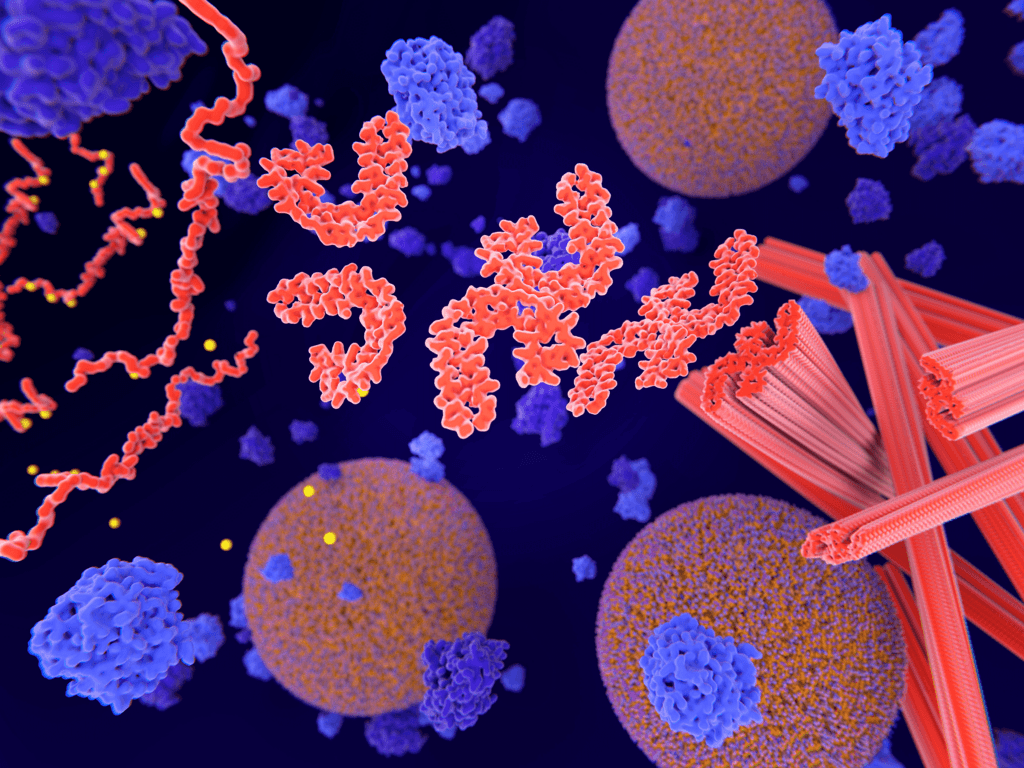
The drug targets amyloid plaque in the brain. The sticky deposits are considered “a key pathological hallmark of Alzheimer disease,” according to Eli Lilly’s study published by the Journal of American Medicine (JAMA).
In the phase 3 study, donanemab was shown to slow cognitive and functional decline by as much as 35% for patients with early Alzheimer’s symptoms.
Furthermore, study participants at the earliest stage of disease saw as much as 60% slowing of decline compared to those who received the placebo. In participants under age 75, the drug slowed decline by 45-48%, and in patients 75 or older, by 25-29%.
“These results demonstrate that diagnosing and treating people earlier in the course of Alzheimer’s disease may lead to greater clinical benefit,” said Liana Apostolova, M.D., of the Indiana University School of Medicine. “The delay of disease progression over the course of the trial is significant and will give people more time to do such things that are meaningful to them.”
A potential barrier to access
Eli Lilly filed the submission to the U.S. Food and Drug Administration (FDA) for traditional approval last quarter. The company said they expect the approval could come by the end of the year.
“If approved, we believe donanemab can provide clinically meaningful benefits for people with this disease and the possibility of completing their course of treatment as early as 6 months once their amyloid plaque is cleared,” said Anne White, EVP of Eli Lilly and President of Lilly Neuroscience.
However, even with traditional approval, barriers to access remain. Centers for Medicare and Medicaid Services (CMS) recently announced that Medicare would only cover this class of amyloid-targeting Alzheimer’s drugs if they receive traditional approval AND patients participate in a registry.
“The best way to permanently ensure timely and affordable access is for CMS to open a reconsideration of its [National Coverage Determination]—as it has promised to do in conjunction with new clinical evidence that is now available—and cover new Alzheimer’s medicines and diagnostics to FDA label,” said a statement from Eli Lilly.
The Alzheimer’s Association previously called the registry requirement “an unnecessary and potentially harmful barrier.”
Amyloid PET diagnostics advance
July 17 was a busy day for Alzheimer’s news. Additionally, CMS announced a proposed National Coverage Determination (NCD) on amyloid positron emission tomography (PET) diagnostics, which an Eli Lilly representative called “another important piece of the treatment puzzle.”
In the memo, CMS proposes to permit Medicare coverage for PET beta amyloid imaging, a minimally invasive diagnostic.
“While amyloid may have normal functions in the body and brain, abnormal amyloid is the first known physiological change found in AD patients, giving rise to the amyloid cascade hypothesis,” explains CMS. “[W]ith the recent development of treatments directed against amyloid, the PET scan would help to confirm the presence of brain amyloid, to alter the course of treatment for the patient and to demonstrate treatment results. In addition, the PET AB can be used to better select patients for AD trials such antiamyloid treatment trials.”
Eli Lilly said they are “encouraged” by the decision. “The clinical value of beta amyloid PET has been demonstrated extensively and consistently over the past decade, and we are pleased to see CMS’s recognition of this in its proposal. Appropriate access to diagnostics is critical to advancing patient care in Alzheimer’s disease, and we look forward to further engaging the agency on this important step forward,” said a statement.