Drug development in the rare disease space has seen a vast amount of innovation in recent years, with a number of groundbreaking therapies coming to market. Yet, the unmet need remains high.
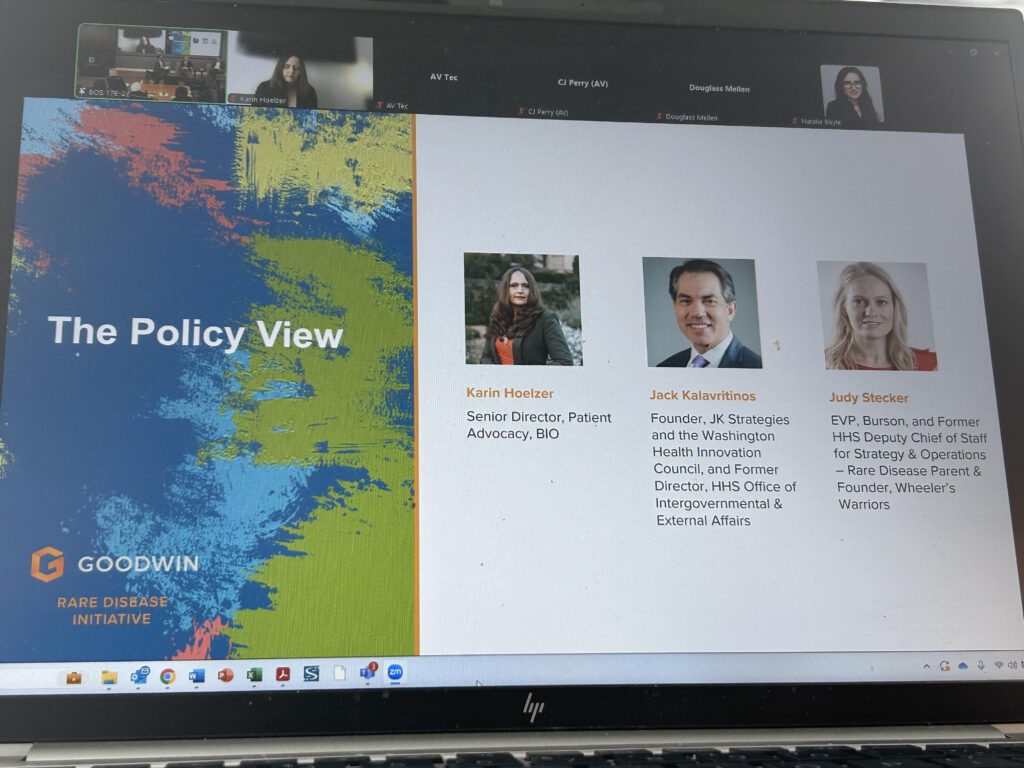
“There are more than 10,000 rare diseases, and almost none of them have treatments,” said Karin Hoelzer, Senior Director of Patient Advocacy at the Biotechnology Innovation Organization (BIO) at the Goodwin Rare Disease Symposium on February 5 in Boston. She spoke on the Policy View Panel, which featured inside-the-Beltway experts with strong ties to the rare disease community.
“There’s so much opportunity,” she added, “but there’s also so much unmet need.”
Patient advocates continue to work to ensure that rare disease development stays strong through investment, political support, and regulatory certainty from administration to administration. That commitment continues in 2025 as patient advocates and policy professionals work to understand the Trump administration’s executive orders and plans for the future.
“Biotech is vital to national security and to the economy, and what we are seeing in particular in the rare disease space is really that it is taking longer and longer to stand up clinical trials, to develop products, and to bring them to market successfully. And with the huge unmet need that we’re seeing in the rare disease community, that is a growing problem,” explained Hoelzer.
ORPHAN Cures Act and solutions to the Inflation Reduction Act (IRA) challenges
Companies and patient organizations are creating and enacting game plans for the new policy landscape, as well as continuing to push long-standing legislative priorities. Luckily, there has already been some positive movement for rare disease legislation.
“Just today, we saw the reintroduction of the ORPHAN Cures Act,” Hoelzer noted, which “helps protect really vital rare disease drug development incentives.”
The Inflation Reduction Act (IRA) exempts orphan drugs from drug price negotiations only if they are approved to treat just one rare disease—a move that BIO says has a chilling effect on the drug development pipeline. The ORPHAN Cures Act would change the IRA’s incentive structure to encourage follow-on development, meaning development for more than one indication.
Orphan drug development also took a hit with the IRA’s “pill penalty,” which created an arbitrary distinction between biologics and small molecule drugs. Currently, the IRA allows for a 13-year exemption from price controls for biologics and just nine years for small molecule drugs.
To remedy this, BIO and patient organizations have been working to pass the EPIC Act.
“The EPIC Act would address the pill penalty and the difference between the time until negotiation eligibility between drugs and biologics,” Hoelzer said.
Another key priority: The Maintaining Investments in New Innovation (or MINI) Act, which Hoelzer explained maintains incentives specifically for the research and development of “genetically targeted therapies,” which are often categorized as small molecules, aiming to give them more favorable treatment under the law similar to biologics.
Accelerated Approval drug reimbursements under Medicaid
Particularly for rare diseases, the Accelerated Approval Pathway is an important tool for getting necessary drugs to patients with unmet medical needs quickly. Yet, there have been a number of issues when it comes to the reimbursement of these drugs by Medicare, Medicaid, and private insurers.
In February 2023, the Centers for Medicare & Medicaid Services (CMS) proposed a model to reduce Medicare payments for accelerated approval drugs, much to the consternation of patients. However, after further analysis and advocacy efforts, CMS decided not to pursue this model.
Panelists agreed that ending the decreased Medicare payments for accelerated approval drugs was positive as there had been concerns that it set a dangerous precedent between coverage for drugs that came to market under accelerated approval versus standard approval.
“We know how vitally important it is for so many of our patient communities to have access to products two to three years sooner than they otherwise would,” said Hoelzer. “Most of our patients just don’t have time to wait.”
Pediatric Priority Review Voucher Program
Another BIO priority is reauthorization of the Pediatric Priority Review Voucher.
“Under this voucher program, a sponsor who receives an approval for a drug or biological product for a rare pediatric disease may qualify for a voucher that can be redeemed to receive priority review for a different product. The sponsor may also transfer or sell the voucher to another sponsor,” explains the Food and Drug Administration (FDA).
“The Pediatric Priority Review Voucher Program is really vital for many of our companies, and I know it is tremendously important for many in the rare disease community,” said Hoelzer. “Unfortunately, the program has lapsed, so we have to get that reauthorized as quickly as possible.”
As the National Organization for Rare Disease has explained, the Rare Pediatric Disease Priority Review Voucher (RPD PRV) program has helped spur rare disease drug development in pediatric populations and brought over 50 therapies to market with critical safety and dosing data specific to children.
Regulatory certainty and the patient perspective
Overall, the policy discussion at Goodwin reiterated two themes: the patient’s perspective and regulatory certainty are the big keys to success.
All panelists mentioned the need to include the patient voice in any legislative or regulatory discussion, as many working on Capitol Hill may not be aware of the minutia of these patients’ needs.
We saw last year with the drug price “negotiations” under the IRA that the patient perspective helped provide context to regulators and legislators, Hoelzer said, adding that a major priority for BIO and patient groups is to ensure patients can navigate the process of providing their perspectives and sharing their stories with organizations like CMS. This is a critical part of BIO’s work to advance necessary improvements in the “negotiation” program to help mitigate the damaging effects of the IRA on access and innovation.
On the legislative and regulatory side, the market has been clear: regulatory predictability is paramount when it comes to ensuring a healthy development pipeline. The problem is that many of today’s policies are impacting the drug development pipeline upstream, eroding the incentives that have made rare disease drug development feasible and risking decades-long cascading effects. As the panel concluded, each participant voiced their commitment to addressing these challenges in 2025.
Hoelzer expressed optimism and reaffirmed BIO’s commitment to partnering with the rare disease patient community to advance policies that support innovation and patient access.