Childhood vaccination rates get a lot of attention, but it’s equally important to work on adult vaccination rates, too.
“Right now, as a number of different pieces of legislation go through implementation, it’s theorized that 9 out of 10 Americans will have no out-of-pocket costs for vaccinations,” said Thomas Acciani, Ph.D., Director of U.S. Vaccine Policy at GSK, in an exclusive interview with Bio.News. “That leaves 10% that still are vulnerable, and that would be in the uninsured population.”
For August’s National Immunization Awareness Month, Bio.News sat down with GSK’s Dr. Acciani to discuss how data and policy, as well as private and public entities, are partnering to close the vaccine access gap —and what work still needs to be done.
Problem-solving vaccine access with data
“One thing that is very important to GSK is using data as a foundation to back policy,” said Acciani. “During the COVID pandemic, we looked at internal IQVIA data that showed a decrease in vaccination rates.”
GSK and IQVIA’s Vaccine Track made public important data dating back to January 2020. The platform allows users to:
- Identify vaccination trends for adults 19+ in the U.S. across multiple vaccines;
- Scan immunization claims data nationally and sub-nationally across years;
- Track trends based on 2019 pre-COVID-19 baseline vaccination uptake; and,
- Highlight where differences exist based on demographics (e.g., age, race/ethnicity, gender, payer type).
“Our goal for Vaccine Track is to support the return to pre-pandemic vaccination rates for adults and to go beyond by empowering the vaccine and public health community with frequently updated, actionable information to get ahead of disease together,” said Judy Stewart, GSK Senior Vice President and Head of U.S. Vaccines.
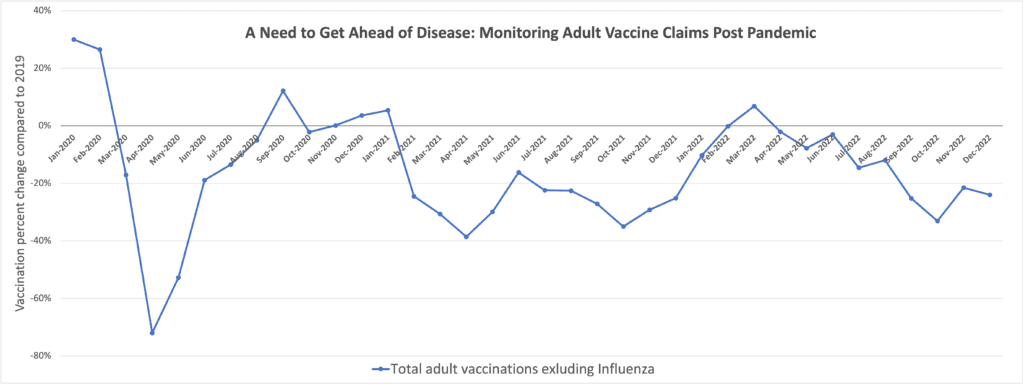
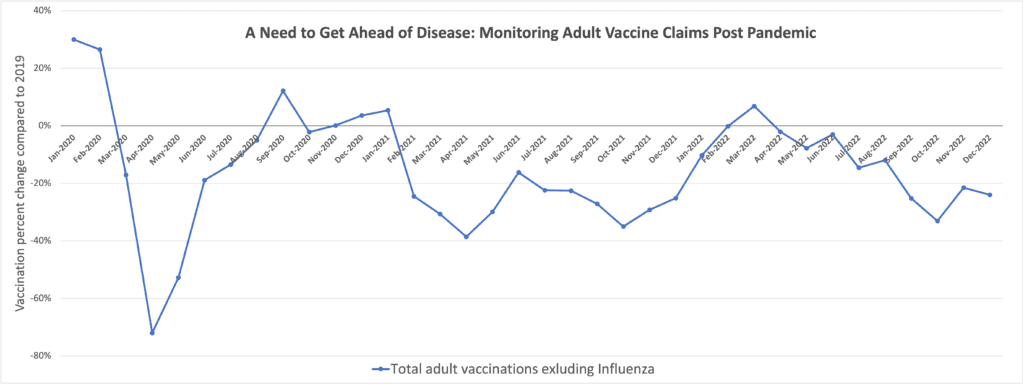
According to GSK’s data, from 2019-2021, there was an 18% decrease in vaccinations for diseases like the flu in adults over 19. By 2021, “nearly half of the states in the U.S. were facing greater than 30% reductions in overall claims for recommended vaccines from 2019 pre-pandemic levels.”
Minority populations were the worst hit: “For Medicare, analysis found more than 30% reduction in overall claims for recommended vaccines among Black and Hispanic populations between 2019 and 2021. This highlights the significant potential impact and exacerbation on disparities in immunization rates in Medicare due to the pandemic.”
Vaccine Track was one step among many that companies like GSK (and others) took to repair disparities in access and vaccine hesitancy in vulnerable populations.
How recent policy is addressing adult vaccine access
The federal government has taken key steps post-COVID to close the vaccine access gap, as well.
Recently, lawmakers appropriated billions of dollars to make vaccinations free to American adults, even as the COVID public health emergency ends.
The 2022 Inflation Reduction Act (IRA) “eliminates cost-sharing for adult vaccines covered under Medicare Part D and expands coverage of adult vaccines under Medicaid and the Children’s Health Insurance Program (CHIP),” writes the Center for American Progress.
Additionally, the Helping Adults Protect Immunity (HAPI) Act, which passed via the IRA, is set to be implemented on October 1. The bill will expand access to adult immunizations by eliminating cost-sharing for vaccines recommended by the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP).
Other bills are in the pipeline, like the Protecting Seniors through Immunization Act. This bill “would provide Medicare beneficiaries access to all recommended vaccines at no additional cost, including shingles and tetanus, diphtheria, and pertussis (Tdap),” explained U.S. Sen. Tim Scott, who helped write the bill. Immunization coverage currently varies by vaccine under Medicare.
“Now, in the post-COVID era, we’ve seen that bills like the Inflation Reduction Act are an effective, larger vehicle to get legislation like the Protecting Seniors and the HAPI Act through so they can really start to tackle the bigger barriers to access such as the financial barriers,” said Acciani. “If you remove the financial barriers, you still have some other issues that need to be addressed, but you’ve addressed one of the biggest ones out there.”
Lastly, “in the President’s budget for Fiscal Year 2023 and 2024, there was the Vaccines for Adults program, also called the Vaccine Safety Net,” explains Acciani. “That would remove another financial barrier for that last 1 out of 10 uninsured Americans.”
The President’s budget articulates “a vision for a Vaccines for Adults program, making immunization infrastructure investments, extending VFC to all children younger than the age of 19 enrolled in Children’s Health Insurance Program (CHIP), and consolidating vaccine coverage for older adults under Medicare Part B,” writes Health Affairs.
While data and policy are key steps when it comes to closing the vaccine access gap, seasoned vaccine advocates like Acciani know there is still more work to do across the private-public spectrum—particularly in the realm of community outreach and education.
Vaccine advocacy is a community endeavor
In June 2023, GSK launched the COiMMUNITY Initiative, “a multi-pronged initiative…to talk about tangible implementation for increasing vaccination rates. It also includes funding and expanding Vaccine Track’s public data—because everything we try to do is based in data, and we use that as a foundation for our policy initiatives.”
Data transparency, combined with a funding commitment of up to $1 million, allows GSK to partner with grassroots healthcare groups to amplify COVID-era successes and maintain momentum in the post-COVID era.
“A silver lining of the pandemic,” said Acciani, “was a decrease in the inequities that have long been part of adult vaccination coverage rates.”
“The U.S. government removed one of the largest barriers to vaccine access: the financial barrier,” he said.
But now, we’re approaching what he called a “COVID funding cliff.”
“State and local groups were really the ones that were the backbone of the success for vaccine uptake. The fear is that as the funding dries up, we are going to lose the lessons learned and all the work that’s been done during the pandemic to get us through it. GSK’s COiMMUNITY initiative will hopefully reduce the effect the impending COVID cliff is going to have by connecting with local organizations and making sure we have the connection and resources needed to address these issues in the future.”
Looking ahead, one role for the industry could be leading a pragmatic reevaluation of how the system works for patients.
“GSK is sharing some of the resources that we’re developing concerning the compressed seasonal window for vaccinations in adults,” explained Acciani. “There’s a very compressed window in the fall for all vaccinations, not just the seasonal ones—it’s for all vaccines.”
“Can we operationalize that schedule in a way to use the whole calendar and bring vaccines out of that space at the end of the year so the fall vaccine season isn’t so crowded?” he asked. “It helps to have non-seasonal vaccines, like shingles, which can be given any time of the year, spread throughout the year when they’re not competing with other more seasonal vaccines, like flu.”
To put it another way, the idea could be to reimagine the adult vaccine schedule similar to the pediatric vaccine schedule.
Suffering from success
Many of the conversations around vaccines—politically, industrially, and socially—reflect a fundamental healthcare paradox.
“We are suffering from the success of vaccines in some ways,” Acciani reflected. “There are some physicians who have never seen a measles case, whereas for physicians just 30-40 years ago, that was fairly common. It’s a blessing and a curse because lives have been saved, but because you don’t have the cases in front of physicians there can occasionally be a struggle when it comes to providers pushing certain vaccine schedules.”
This paradox has been seen recently as the world moves beyond the COVID pandemic, yet has failed to build the structures that will allow us to address the next pandemic.
“It’s always easy to say ‘we should have done this’ or ‘we should not have done that,’” said Pierre Delsaux, Director General of the Health Emergency and Preparedness Response Authority (HERA) European Commission at the 2023 BIO Convention. “But it’s only easy to say that after the fact—it’s easy to rewrite history. What’s difficult is for all of us to come together to try to see what the future needs and to try to be prepared for it—and we cannot do it in isolation.”
Recent policies, like the HAPI and Protecting Seniors through Immunization Acts, as well as the additional funding for adult vaccinations in the IRA, are positive steps. But it’s undeniable that, when it comes to pandemic preparedness, industry calls for action are the loudest in the room. And, in many ways, that all starts with ensuring vaccine access for all.
Hinting at the steps companies like GSK intend to take even after implementing their current projects, Acciani noted, “Harmonization amongst the federal policies as it relates to Medicare would also be a huge step in improving adult vaccination access. While the IRA was wonderful at eliminating the financial barrier, for patients, there are still some provider barriers that exist. We know providers are some of the strongest indications of vaccine uptake. So, we want to make sure we support our providers in being able to vaccinate their patients.”




