Top U.S. health officials reported a decline in the growth of new monkeypox cases and outlined the federal response to the outbreak, during a Senate Health, Education, Labor and Pension (HELP) Committee hearing Wednesday.
The committee made it clear they expected meaningful progress in the effort to combat the monkeypox emergency. “COVID was never going to be the last public health crisis we face and neither is monkeypox,” said Sen. Patty Murray (D-WA), Chair of the HELP Committee. “I don’t want to just hear today about the steps you will be taking. I do want to see action.”
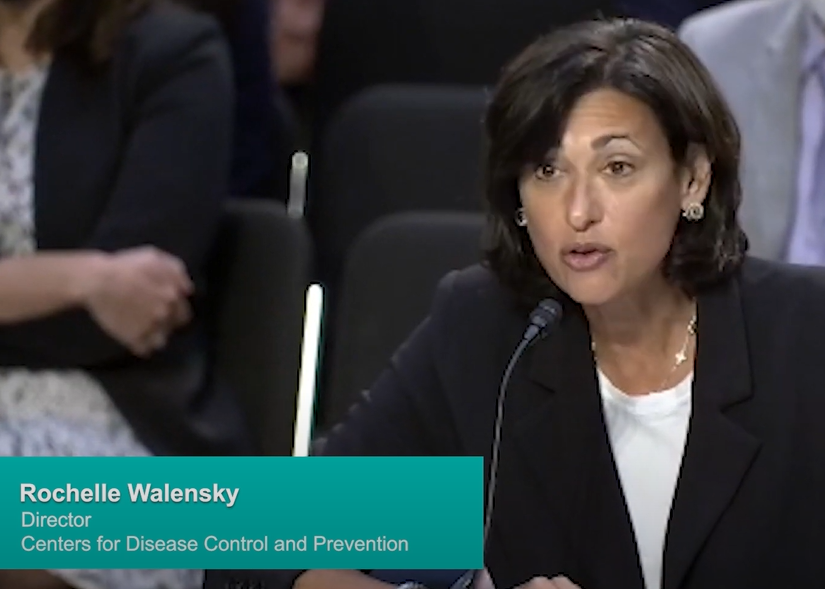
CDC Director Rochelle Walensky offered some positive news. “Over the last several weeks, we’ve been pleased to see a decline in the growth of new cases here and abroad, though there are areas in the United States where the rate of rise in new cases is still increasing,” she said. “We approach this news with cautious optimism, recognizing that we must continue to aggressively respond with our entire toolkit, including vaccination, testing, and education about risk, to inform behavior change.”
While the monkeypox outbreak has shown that public health officials still struggle with addressing health emergencies, Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases at the National Institute of Health, said they have gained useful experience from past challenges.
“Lessons learned during the response to AIDS and COVID-19, such as avoiding stigma and ensuring the medical countermeasures get to where they are needed most, should help us in our efforts to respond to the ongoing monkeypox emergency,” Fauci told the hearing. “In addition, the U.S. response to monkeypox should help to inform our response to the inevitable next emerging or reemerging infectious disease of pandemic potential.”
Phyllis Arthur, BIO’s Vice President of Infectious Disease and Emerging Science Policy, explained the importance of supporting the systems and industry that develop and supply the medical technology we need to combat pandemics, epidemics, and public health emergencies.
“I think that we’ve now had multiple infectious disease crises in a row and we are learning from each of these, but it’s really important to invest in systems and actually sustain funding for the routine public health activities, which is the foundation for our ability to respond in an emergency,” Arthur said. “If those systems are weakened, if they’re not reinforced and sustained with funding, if those people are not there, then we do have these failures of the ability to respond from one emergency to the other.”
Video: Highlights of the hearing
Transcript of the video
The following is a transcript of what is said in the video above:
U.S. Senator Patty Murray (D-WA), Chair of the Senate Health, Education, Labor and Pensions (HELP) Committee: COVID was never going to be the last public health crisis we face and neither is monkeypox. The question is not whether there will be a new threat, it is when it will strike and whether we will be ready. The truth is the monkeypox response so far has not been encouraging. But there are some clear signs of progress and there are clear steps that we can and should take to improve. And I don’t want to just hear today about the steps you will be taking, I do want to see action.
U.S. Senator Richard Burr (R-NC) Ranking Member of the Senate Health, Education, Labor and Pensions (HELP) Committee: I’m glad that we’re finally having a hearing on the monkeypox outbreak as it hits our nation. While monkeypox is now a public health emergency, it didn’t have to become one. I think the one promising thing that can be said this morning is the infection rate has slowed. That may be the only thing since May, when the first transmission was recorded in the UK, Europe.
Rochelle Walensky, Director, Centers for Disease Control and Prevention: Over the last several weeks, we’ve been pleased to see a decline in the growth of new cases here and abroad, though there are areas in the United States where the rate of rise in new cases is still increasing. We approach this news with cautious optimism, recognizing that we must continue to aggressively respond with our entire toolkit, including vaccination, testing, and education about risk to inform behavior change.
Robert Califf, Commissioner, Food and Drug Administration: The FDA has been actively working with our government and private sector collaborators to respond to the continuing public health threat since the first monkeypox case came to the US. We’ve been working diligently to help ensure access and proper information regarding vaccines, diagnostics, and treatments for those who need it most.
Dawn O’Connell, Assistant Secretary, Administration for Strategic Preparedness and Response: We continue to maintain our smallpox preparedness—that’s critical. Our frontline vaccines continue to be available and have not been impacted by our monkeypox response. But we have added the capability to be able to provide the JYNNEOS vaccine to those that are immunocompromised in the case of a smallpox outbreak. And we are evaluating with each dose that we make available to the monkeypox outbreak what it means for that preparedness and smallpox
Anthony Fauci, Director, Institute of Allergy and Infectious Diseases, National Institute of Health: Lessons learned during the response to AIDS and COVID-19, such as avoiding stigma and ensuring the medical countermeasures get to where they are needed most, should help us in our efforts to respond to the ongoing monkeypox emergency. In addition, the US response to monkeypox should in turn help to inform our response to the inevitable next emerging or reemerging infectious disease, of pandemic potential.
Phyllis Arthur, Vice President, Infectious Diseases and Emerging Science Policy, BIO: I think that we’ve now had multiple infectious disease crises in a row and we are learning from each of these, but it’s really important to invest in systems and actual sustain funding for the routine public health activities, which is the foundation for our ability to respond in an emergency. If those systems are weakened, if they’re not reinforced and sustained with funding, if those people are not there, then we do have these failures of the ability to respond from one emergency to the other. And so we aspire to really have been advocating strongly for sustained increased and sustained funding for both the public health community but also the work that happens within the aspr for medical countermeasure development and procurement and sustainment. And the surveillance and other capabilities that’s so core to the CDC. Those two areas need to be robust, and they need to be continuous because we never know when we’ll have multiple emergencies sitting on top of each other as we do now.