With the deadly threat of drug-resistant infections increasing daily, we desperately need actions to address the broken commercial marketplace for novel antimicrobials—including the PASTEUR Act, a novel pull incentive, and reforms to antimicrobial reimbursement—said a CEO speaking on behalf of the Biotechnology Innovation Organization (BIO) and the Antimicrobials Working Group (AWG) at a July 11 Senate hearing.
The natural progression of antimicrobial resistance has been accelerated by over-reliance on antibiotics, participants told the Senate Health, Education, Labor, and Pensions (HELP) Primary Health and Retirement Security Subcommittee during a hearing titled “Superbugs: The Impact of Antimicrobial Resistance (AMR) on Modern Medicine.”
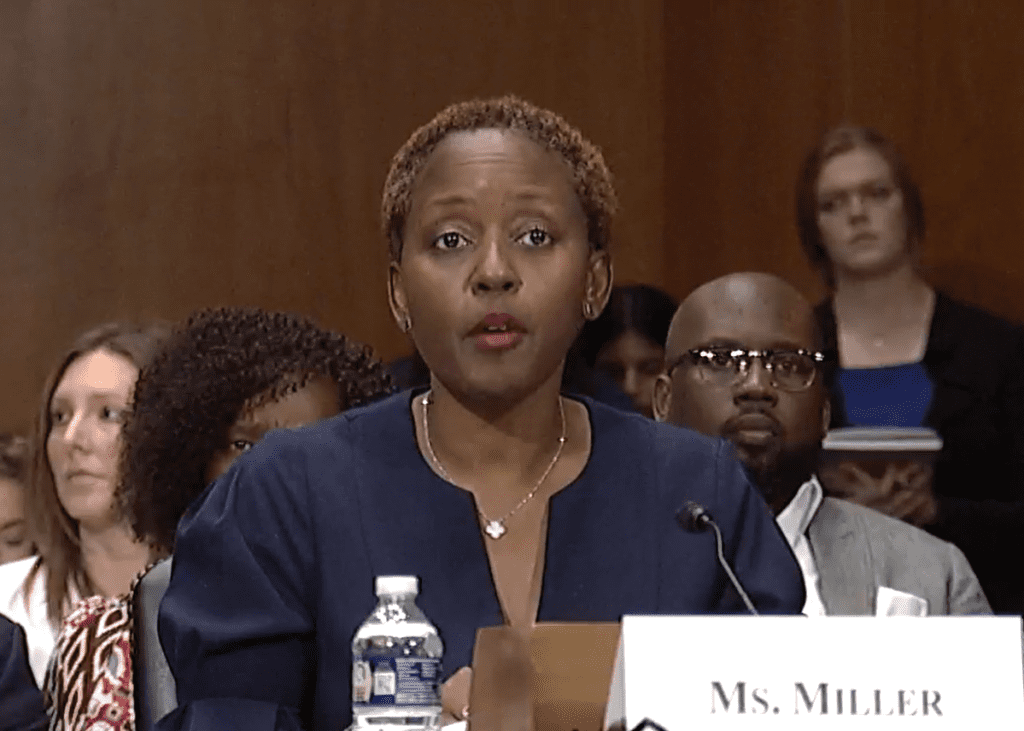
“Bacteria and fungi adapt and evolve over time and become resistant to these treatments—a phenomenon known as antimicrobial resistance (AMR),” said Christine Ann Miller, CEO of BIO member Melinta Therapeutics and chair of the Antimicrobials Working Group. “Overuse and misuse of current antibiotics accelerates AMR. For example, in the outpatient settings, the CDC (Centers for Disease Prevention and Control) estimates that one-third of antibiotics are used improperly.”
We have benefited greatly from antibiotics, but unless we support development by addressing weaknesses in the market those benefits are now under threat, Subcommittee Chair Sen. Ed Markey (D-MA) said in his opening remarks. “More than 100 years ago, the discovery of antibiotics revolutionized modern medicine. Antibiotics alone have extended our average lifespan by 23 years. But the rise in antimicrobial resistance threatens to undo 100 years of medical progress,” he said.
An emergency ‘here and now’
Miller explained the urgency of the problem. “This rise in AMR is rapidly rendering our antimicrobial arsenal ineffective and represents a problem in the here and now—it will also continue to get progressively worse over time. As AMR becomes more prevalent, many medical procedures that are commonplace today will become too risky to undertake, with catastrophic consequences to medical care, including death,” she said.
The numbers across the healthcare spectrum are stark, Ranking Member, Sen. Roger Marshall (R-KS) explained in his opening remarks. “Three million Americans this year will get some type of an antimicrobial resistance superbug,” he said. “One hundred Americans will die today. One hundred will die tomorrow, and every day this year from some type of [an antibiotic] resistant bug.”
Melanie Lawrence, a healthcare advocate with the Cystic Fibrosis Foundation, offered a first-person perspective. She has been taking antibiotics her whole life to manage her cystic fibrosis. “Now in my forties, the bacteria in my lungs are resistant to nearly all antibiotics except for Tobramycin, which I cannot take because it is so toxic to my already-damaged kidneys and hearing,” she said. “My focus is now on managing my symptoms and maintaining the best quality of life possible.”
We urgently need new antimicrobials, she said.
“Private sector investments alone won’t solve the problem. We need the federal government to lead and support innovative policy solutions with an all-of-the-above approach to help people like me live long enough to see our children thrive. Personally, I want to see my son graduate college or even become a grandparent—something I’ve never even allowed myself to imagine because it feels so out of reach without new antibiotics.”
A broken commercial marketplace
Miller broke down the problem with the broken antimicrobial marketplace which she said is unique to this area of medicine. There is no problem with innovation, science can come up with new antimicrobials, but the way we use antimicrobials, and the need to use them sparingly, means that drug developers lose money if they invest in antimicrobials, she said. Meanwhile, flaws in our reimbursement system mean that hospitals have a financial incentive to withhold the newest antimicrobials.
“What remains is a commercial marketplace problem underpinned by systemic post-approval and reimbursement challenges which must first be acknowledged, and then corrected,” Miller said.
She called for legislation to address the problem.
There has been some legislation and policy initiatives, as Dr. Helen Boucher, Dean and Professor of Medicine at Tufts University School of Medicine noted. She pointed to the passage of “the Generating Antibiotic Incentives Now (GAIN) Act in 2012 and enactment of the Limited Population Antibacterial Drug (LPAD) review mechanism in 2016 as part of the 21st Century Cures Act, which helped improve the regulatory environment for the study and evaluation of new antibiotics and antifungals to address unmet needs in limited patient populations.”
Additionally, Boucher said, “the National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) was launched in 2015 and provided an important framework for a coordinated, comprehensive federal response to AMR. The second iteration of the plan was released in 2020 and largely aims to build upon the progress made since 2015.”
But Miller said more needs to be done.
“Passage of the GAIN Act was intended to spur antimicrobial innovation. However, it has fallen short in pulling novel drugs to approval, and even more importantly, ensuring patients have access to those drugs once they are approved,” she said.
“The federal government also implemented additional incentives to support the research and development of new drugs,” said Miller, “such as the CARB-X program under the Biomedical Advanced Research and Development Authority (BARDA). These programs have been resoundingly successful in their mission and have become vitally important to antimicrobial development.”
Passing the PASTEUR Act
Miller, and others in the hearing, promoted passage of the PASTEUR Act, which would create an alternative payment mechanism that decouples payment from the volume of antimicrobials used, creating an incentive for drug developers that pursue R&D of innovative antimicrobials. BIO is a strong supporter of the PASTEUR Act. Miller also noted the need for antimicrobial reimbursement reform to ensure patient access to novel therapies.
At the hearing, Sen. John Hickenlooper (D-CO) maintained that antimicrobial drug development has not kept pace with drug resistant pathogens, largely because of the lack of financial incentives. He asserted that the PASTEUR Act helps incentivize investment in antimicrobial innovation by reducing market uncertainty, which encourages more scientists to devote their careers to the problem.
Miller agreed, and said people are not entering the infectious disease field due to limited financial opportunities.
“We need to address the commercial marketplace. This is definitely something that really needs the federal government to step in and address,” said Miller. “We need to see reforms and reimbursement. We need to see incentives like the PASTEUR Act be put in place so that all the development of public-private partnerships that are happening today, actually have a place to land and that patients can get the life-saving medicines that they need.”