Concerns over sepsis, a life-threatening reaction to infections, are on the rise. And growing antimicrobial resistance (AMR) is making the condition harder to treat. Additionally, it’s difficult to diagnose in children and infants, who also carry a higher susceptibility rate. During Pediatric Sepsis Awareness Week (April 16-22), we explore these challenges and potential solutions.
What is sepsis?
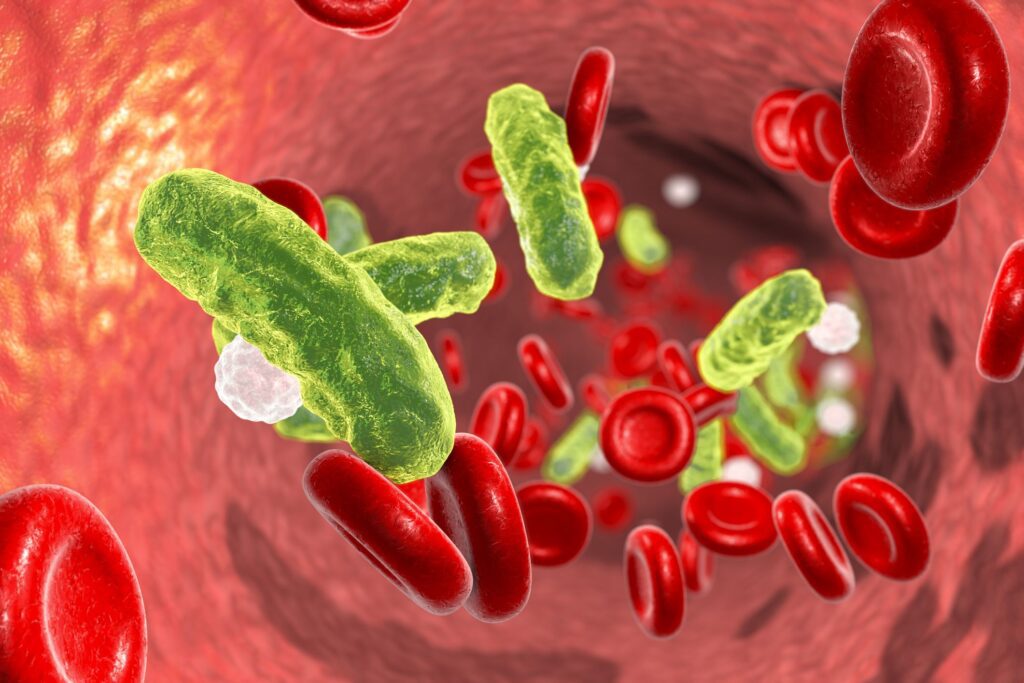
Sepsis, also known as septicaemia or blood poisoning, is an emergency condition where the body reacts in a deadly way to a severe shock from an infection. Known as “septic shock” when it reaches an alarming stage, the condition can cause severe problems from organ failure to tissue damage—and even death.
Common symptoms of sepsis include but are not limited to:
- Fever and chills
- Confusion or disorientation
- Rapid heart rate and breathing
- Low blood pressure and weak pulse
One important factor about sepsis is that it’s a secondary medical condition, emerging from an initial infection that has worsened. Thus, symptoms may mimic the first medical condition, and the development of sepsis may go unnoticed.
Currently, no single definitive test for a diagnosis exists. Medical professionals utilize a variety of testing and examinations, such as blood and urine tests, x-rays, and monitoring key sepsis biomarkers (like C-reactive protein and procalcitonin).
Typically, the individuals with a higher chance of developing sepsis are those who are at a vulnerable age, like the very young or old; have an existing chronic condition; and are hospitalized patients.
The Biotechnology Innovation Organization (BIO) has not only raised awareness about this illness through many informative articles, but numerous BIO members are actively fighting against sepsis via various initiatives.
Why is pediatric sepsis more dangerous?
Premature babies, infants, and children of all ages are more susceptible to sepsis for various reasons. In fact, in 2017, children accounted for more than half of all sepsis cases worldwide (especially neonates), as stated by a report from The Lancet.
Although there are similarities in sepsis among children and adults, children have many varying experiences due to their differences in age and body functions and abilities (such as hemoglobin concentration, blood pressure, heart rate, protein mass, and more). These factors also account for more challenging diagnoses in children.
Infants are particularly more at risk due to their developing immune systems. Additionally, they can also carry over the infection from their mothers following birth, known as neonatal sepsis.
Socioeconomic factors also play a role in determining pediatric sepsis treatment outcomes. According to UC Davis Health, “Preterm infants who are Black are 13 times more likely to develop sepsis and 15 times more likely to die than non-Black infants.” This may be due to low income and a lack of health insurance, both of which are proven to cause more infant deaths from sepsis.
Why is antimicrobial resistance a threat?
In children and adults alike, there’s a higher chance of developing sepsis while being treated at a hospital. In infants, one reason for this is the long-term use of catheters or other medical devices.
However, the resistance to antibiotics (especially in hospital-induced illnesses) is a threat to infection treatments. In fact, many sepsis cases, including pediatric sepsis cases, in hospitals begin or worsen due to AMR responses from patients.
As AMR continues to advance, it can not only lead to more fatalities caused by sepsis, but increases the risk of patients in general. Despite the condition patients come in for (such as a urinary tract infection or a burst appendix), they all equally have the same risk of developing sepsis.
Although a fatal illness, there are simple steps that can be adapted for sepsis prevention. The methods can be broken into two categories, as highlighted by WHO:
- Prevention in communities: Incorporate strong practices of strong hygiene and sanitation (such as in food preparation or hand-washing) and increase access and use of vaccines.
- Prevention in medical facilities: Embodying exceptional infection prevention and control (IPC) programs and stressing hygiene and sanitation for cleaner equipment and overall working environment.