In an effort to speed drug development, the Food and Drug Administration (FDA) often allows the use of biomarkers to help prove whether new drugs work. But what are biomarkers, and how do they work?
Let’s take a look.
Biomarkers enable Accelerated Approval for promising new drugs, and the U.S. Food and Drug Administration (FDA) wants to use biomarkers to speed the development of new gene therapies.
As defined by the FDA, a biomarker is a “specific measurable characteristic that acts as an indicator of normal biological processes, pathogenic processes, or responses to either an exposure or intervention.”
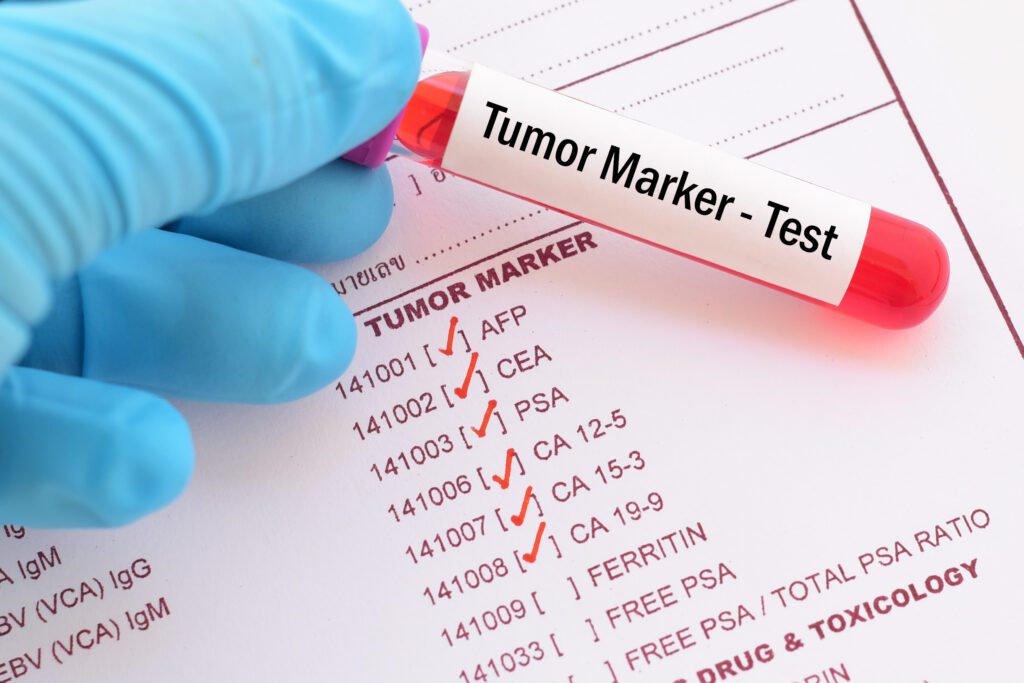
Biomarkers, or biological markers, are measurable indicators within bodily fluids, tissues, or genetic material. They can be proteins, chemicals, or a product of their interaction with a target molecule or cell.
Biomarkers act as clues given by the body’s biological systems, offering a glimpse into cellular processes, organ function, and the progression of disease. They play an essential role in research and clinical practice as they contribute to early disease detection and assess the efficacy of treatment. In specific cases, biomarkers assist in identifying an accurate diagnosis and formulating a personalized treatment plan.
What are biomarkers?
There are many types of biomarkers.
The FDA and the National Institutes of Health (NIH) have selected specific terminology for biomarkers in order to promote a consistent language throughout the scientific and clinical communities. Despite their efforts, there continues to be an abundance of terms that are used within each category which may be considered confusing.
Generally, classification is based on specific characteristics and their clinical applications.
Here are seven of the most widely accepted biomarkers.
1. Diagnostic biomarkers
Diagnostic biomarkers are involved in early detection and the confirmation of a disease. Blood glucose levels, for example, can be used in the diagnosis of diabetes. An elevated PSA (prostate-specific antigen) in the blood may indicate prostate cancer.
2. Prognostic biomarkers
In order to assist with identifying the severity of a disease and the potential course it may take with or without treatment, prognostic biomarkers may be used. Brain natriuretic peptide (BNP) is an example of a prognostic biomarker that, when elevated, suggests prognosis of heart failure. BNP is then used as a monitoring biomarker to guide treatment decisions.
3. Predictive biomarkers
A predictive biomarker determines individuals likely to respond positively to a specific treatment. In clinical practice, it may be used to personalize treatment plans. Breast cancer genes BRCA 1 and HER2/neu are overexpressed in some patients and when present, are predictive for specific targeted therapies. Early recognition of this information offers patients the opportunity for earlier treatment with direct treatment and the potential for improved outcomes.
4. Monitoring biomarkers
A monitoring biomarker is used as a method to assess a disease or medical condition or to track exposure to a medication. The potential for liver toxicity, for example, is measured via a liver function test (LFT). Monitoring serial troponin levels will identify and exclude myocardial infarction.
A biomarker such as PSA may be both a diagnostic biomarker in an unsuspected patient and a monitoring biomarker while undergoing treatment and cancer burden is being assessed and managed.
Opioid levels are used in cases of addiction to monitor compliance.
5. Pharmacodynamic or response biomarker
To indicate the biological activity of a medication to either assist in dose selection or measure a specific response, a pharmacodynamic or response biomarker is indicated.
In the setting of chronic atrial fibrillation or a history of deep vein thromboses, the international normalized ratio (INR) is used to evaluate and assess a patient’s response while on Coumadin.
Within this category is also the surrogate endpoint biomarker, which is used to determine the risks and benefits to individuals based on epidemiology, therapeutics, pathophysiology, and scientific evidence.
As an example of a surrogate endpoint marker, the reduction of blood pressure is associated with a subsequent reduction in the rate of stroke. Along with an overall reduction in mortality, this data has been used as the foundation within clinical drug trials to treat hypertension.
6. Susceptibility or risk biomarkers
In order to determine an individual’s potential for developing a disease or condition they don’t currently have, susceptibility or risk biomarkers come into play. For example, high-risk human papillomavirus (HPV) subtypes are used to establish patients at increased risk of developing cervical cancer.
7. Safety biomarker
If there is a concern about exposure to a specific medication or toxin, a safety biomarker will be used to offer information regarding the likelihood of the exposure and its presence within the individual. As liver function tests may be used as a monitoring biomarker, they are also considered safety biomarkers when used to evaluate hepatic toxicity. Serum creatinine, total protein, and albumin are used to monitor kidney function in the setting of suspected kidney toxicity.
Why biomarkers matter
Biomarkers are a necessary resource that assist and guide the medical and scientific communities through the complexities of both health and disease.
Despite challenges surrounding their categorization and standardization, biomarkers have the potential to revolutionize healthcare by enabling early disease detection, maximizing patient care, and advancing medical science via the advancement of effective drug development.