The Senate Health, Education, Labor, and Pension (HELP) Committee on May 2 discussed Senate Bill 1339, “The Pharmacy Benefit Manager Reform Act,” and three other bills addressing drug costs in the United States, but delayed a vote until May 11.
“The [PBM] Reform Act that I have introduced with Ranking Member Cassidy and senators Murray and Marshall makes some much-needed and long overdue reforms to the system,” said Chair Bernie Sanders (I-VT) as he opened the session. “Under this legislation, PBMs will be required to share more information with employers and insurance plans, pass rebates onto employers and insurance plans and would ban PBMs from charging one price to a pharmacy and another price to an insurance plan and pocketing the difference. It has been estimated that this bill will save close to $2 billion over 10 years, lower health insurance premiums, and will help keep struggling independent pharmacies in business.”
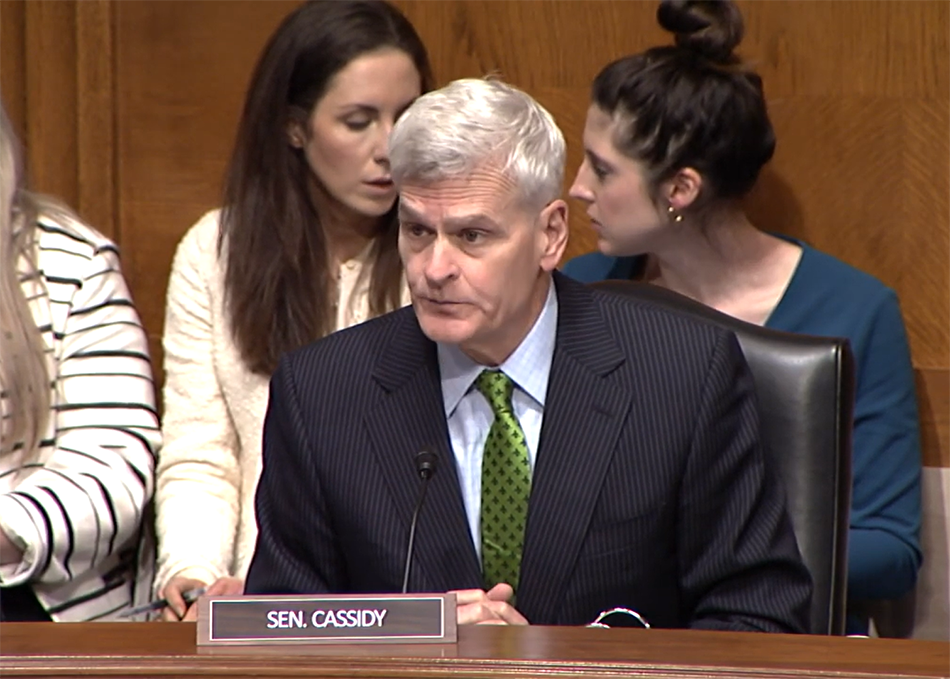
Ranking Member Bill Cassidy (R-LA) said the bill would “bring much-needed transparency to an opaque structure, in which middlemen have some sort of margin—we know not which—at the expense of customers and patients who use the service.” He added that addressing PBM transparency would make it possible to “lower drug costs without overhauling the entire health care system or threatening the ability and incentives to produce life-saving drugs in the future.”
Pharmacy benefit managers (PBMs) oversee prescription drug prices for insurance plans, and they are criticized for driving up drug prices. With three PBMs controlling 80% of the market, they use their market power to negotiate often hefty rebates from drug manufacturers, in exchange for giving insurance coverage for their drugs. But instead of passing on savings to patients, as they are supposed to do, PBMs pocket the savings as profits, research shows.
Markup postponed
After some discussion of procedure and timing, the committee took a recess and returned with Sen. Sanders announcing the markup session would be postponed until May 11.
Sen. Cassidy had expressed concerns in his opening statement that Democrats would be supporting amendments that had been “taken off the table” during negotiations on the legislation, and there was a concern about missing Congressional Budget Office scores, as well as technical support from different administrative agencies on the issue.
Senators also concluded that a markup would be better scheduled after the May 10 HELP Committee hearing to which three PBM CEOs are invited: David Joyner, President of Pharmacy Services CVS Health; Adam Kautzner, President Express Scripts; and Heather Cianfrocco, Chief Executive Officer OptumRx. Senators voiced their desire to see that hearing happen in case there was any additional information that they may not be privy to that might affect their vote.
What the bill would do
Originally introduced April 27, the Pharmacy Benefit Manager Reform Act (S. 1339) is sponsored by Senate HELP Committee Chair Sanders and Ranking Member Cassidy, as well as Sens. Patty Murray (D-WA) and Roger Marshall (R-KA) to bipartisan support.
The legislation would increase transparency for PBMs and mandate that they pass on the rebates they take from drug makers to insurers and employers. The bill would also ban spread pricing, in which pharmacies are charged much more than the price PBMs negotiate for a drug.
The bill is also supposed by a number of employer groups, who wrote a letter to the Committee calling for: a complete and unrestricted transparency into the PBM “black box”; a ban on so-called “spread pricing”; requiring 100% pass-through of rebates, discounts, fees, and other payments from drug manufacturers; and the application of the same fiduciary standards used on employers to PBMs.
What to expect in the coming weeks
Despite the delay there is optimism that the markup and future vote on the bill will get back on track next week in a bipartisan fashion. With additional PBM bills in both the House and Senate, as well as a number of investigations and inquiries into the behavior of PBMs, there is the political will to address the issues.
The trick will be to maintain momentum so that a major bipartisan consensus can happen and effective reform into the PBM system can be implemented so that patients no longer bear the brunt of needlessly high drug costs.